By Laura Friedman
In honor of World Tinnitus Day April 18, Hearing Health Foundation (HHF) wants to draw attention to the effects and challenges associated with tinnitus.
The U.S. Centers for Disease Control estimates some 15% of Americans—about 50 million people—have experienced tinnitus. Roughly 20 million people struggle with chronic tinnitus, while 2 million have extreme and debilitating cases. It is also a top war wound among active U.S. military personnel and veterans.
Tinnitus is defined as the perception of sound when there is no external, acoustic source. Individuals with tinnitus may describe the noise as buzzing, hissing, whistling, swooshing, or clicking. Roughly 90 percent of tinnitus cases occur with an underlying hearing loss.
Tinnitus can be either intermittent or chronic. People who experience intermittent tinnitus occasionally hear sounds in their ears that can last from minutes to hours after being exposed to excessively loud noises. An example would be someone sitting near the fence of a NASCAR race without wearing hearing protection. People with chronic tinnitus, on the other hand, often experience noise more frequently, which can last for more than three months.
The impact of tinnitus on everyday life differs from person to person. Researchers found that most people with chronic tinnitus are not too bothered by it. Many of these people prefer to only see a doctor for assurance that their tinnitus is not an indication of a serious disease or impending deafness. People who were bothered by their tinnitus reported that it was annoying, invasive, upsetting, and distracting in daily life. In a small tinnitus self-help group, some members frequently describe having problems sleeping, understanding speech, poor concentration, inability to relax, and depression.
People with age-related hearing loss, or presbycusis, may also experience a ringing, hissing, or roaring sound in the ears. Presbycusis progresses over time and is generally more severe in men than in women and the risk increases with age, as shown in epidemiological surveys.
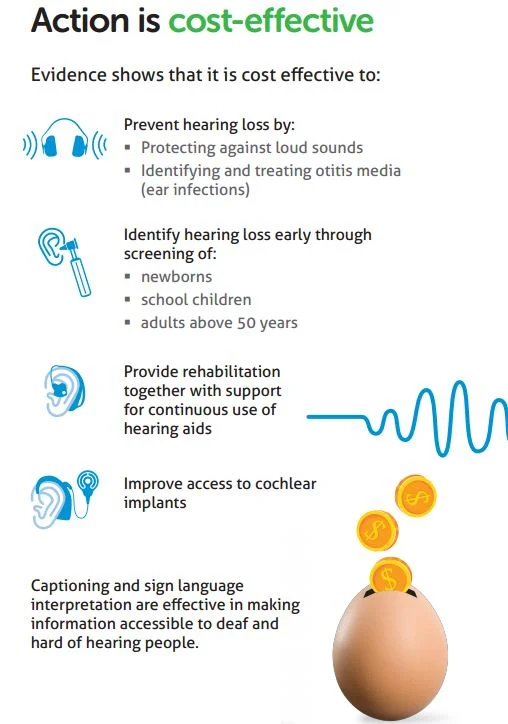
Although there is no cure for tinnitus, there are available treatments that can minimize tinnitus symptoms. Tinnitus Activities Treatment (TAT), cognitive behavioral therapy (CBT), and Tinnitus Retraining Therapy (TRT) are sound therapies that can lessen the effects of tinnitus, often times very helpful in combination with counseling. Furthermore, by using hearing protection and noise reduction technologies, and by avoiding excessive noise, many people can prevent significant hearing problems.
Taking care of your hearing should always be part of keeping healthy overall. If you suspect a hearing loss or tinnitus, HHF recommends getting your hearing checked. If you do have a hearing loss or tinnitus, talk with your hearing healthcare professional about available treatments. For more information, visit hhf.org/tinnitus or email us at info@hhf.org.
Laura Friedman is the Communications and Programs Manager of Hearing Health Foundation.