By Vicky Chan
Like most moms, Brandy has always been a champion for her three sons, Anthony, 12, Andersyn, 10, and Ayden, 7. Her sons are unlike most sons; each has bilateral sensorineural hearing loss and enlarged vestibular aqueduct syndrome.
Brandy’s journey as a parent-advocate had a difficult start. She was completely unfamiliar with hearing loss in children before she became a mother, and accessing proper treatment for the trio was a challenge. Brandy juggled numerous audiologist appointments that were a five-hour round-trip drive from home. And, for her oldest child, Anthony, a hearing loss diagnosis came two years delayed.
Clockwise from left: Ayden, Andersyn, Anthony, and Brandy.
Anthony had typical speech development and passed all his first- and second-year wellness and hearing checks by his pediatrician. When he was 2, Anthony fell and hit his head. Brandy suspected the trauma had caused either hearing loss or a cognitive disorder, but the doctors assured her Anthony suffered no permanent damage and took no action for him.
Brandy’s instincts were correct. When her second child, Andersyn, was diagnosed with hearing loss at birth a few months after Anthony’s head injury, she insisted Anthony receive a detailed hearing evaluation. Born in 2005, Anthony never received a newborn screening despite the passage of the Newborn and Infant Hearing Screening and Intervention Act of 1999, which mandated the practice.
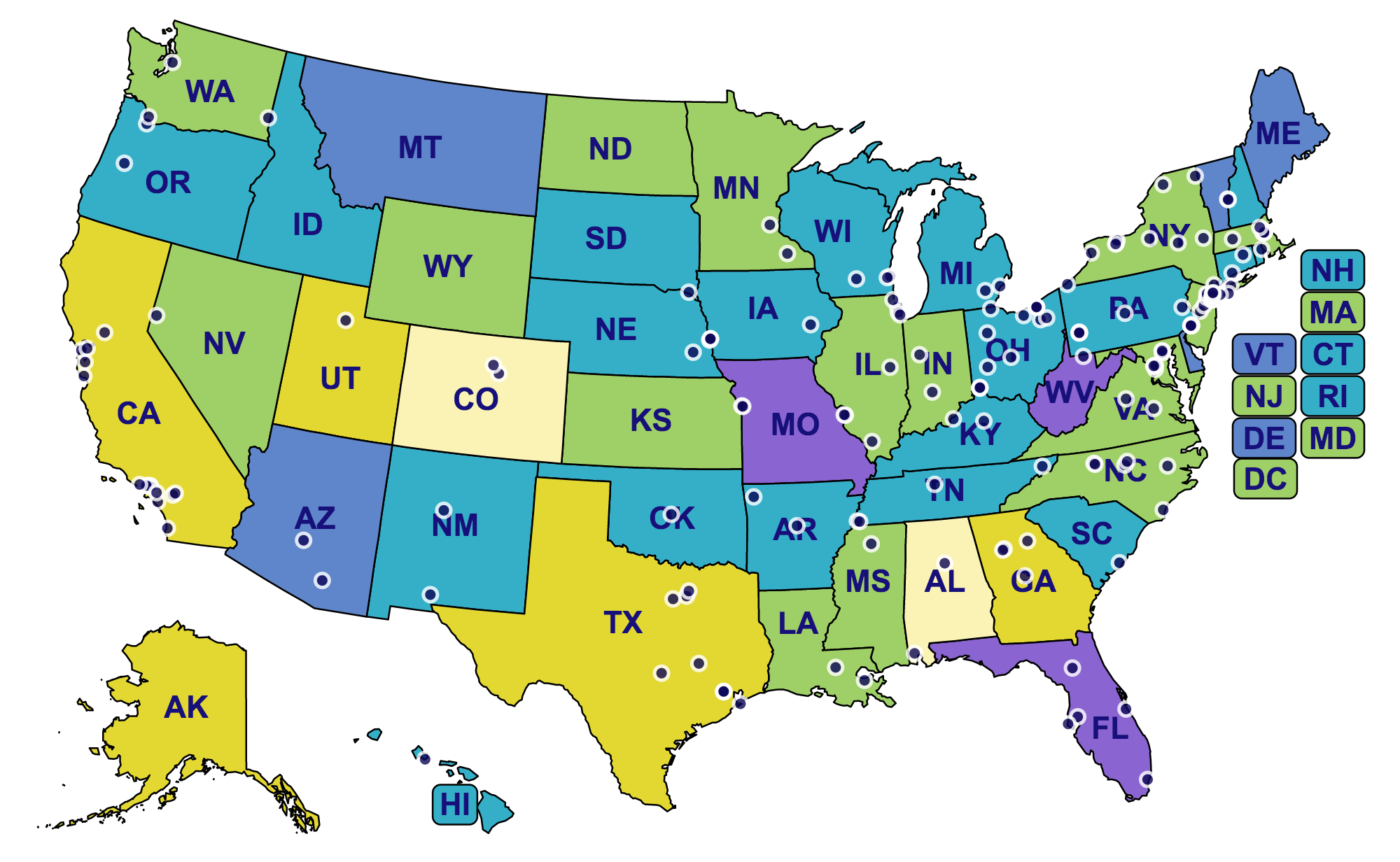
The legislation quickly improved the rate of newborn hearing screening. In 2005, 94.2% of babies in the U.S. were screened, but some states lagged behind. In Tennessee, where all three of Brandy’s sons were born, only 66.9% of newborns were tested—the lowest in the nation. Unfortunately, Anthony was among the 30.1% of Tennessee’s babies not screened. However, by Andersyn’s birth in 2007, the state’s rate increased to 91%. It was only due to Brandy’s perseverance that Anthony was ultimately given a comprehensive exam, diagnosed with severe bilateral hearing loss, and fitted for hearing aids.
Brandy’s message is that newborn screening is vital. “If your child has hearing loss, it is best to start intervention as soon as possible and have your child fitted for hearing aids or cochlear implants if they need them.”
With his hearing aids, Anthony was fascinated by all the new sounds he could hear—including the squishy sound of Brandy’s flip-flops as the pair walked through a parking lot. At that moment, Brandy realized it was likely that Anthony, like Andersyn, was born with hearing loss, but it only became detectable to her after his head injury.
Andersyn was given a newborn hearing test so Brandy knew immediately that he had severe bilateral hearing loss. Later on, one audiologist suggested he wasn’t benefiting from his hearing aids, but Brandy knew differently; with Andersyn’s hearing aids turned up, a sound as subtle as crinkling paper near his ears would startle him. Andersyn now does exceptionally well with hearing aids, as does Brandy’s third and youngest child, Ayden, who was also born with severe hearing loss in both ears. The boys’ doctors have cited a genetic connection of unknown cause.
Today, hearing loss is an ordinary part of life for her three boys, thanks to Brandy’s tireless advocacy. With help from FM systems and speech therapy, Anthony, Andersyn, and Ayden all receive a mainstream education. They enjoy baseball, basketball, hunting, swimming, riding four wheelers, and fishing. HHF’s CEO, Nadine Dehgan, exclaims, “All three boys are incredibly fortunate to have Brandy, a devoted mother who has prioritized their hearing health.”
Anthony, Andersyn, and Ayden are participants in HHF's "Faces of Hearing Loss" campaign.
Receive updates on life-changing hearing research and resources by subscribing to HHF's free quarterly magazine and e-newsletter.