By Maggie Niu
Childhood hearing loss is a (rapidly) growing epidemic. A study performed by the World Health Organization (WHO) found that 60 percent of childhood hearing loss is preventable. If left untreated, the child can experience many health issues such as delayed language development and academic underachievement as well as social isolation, which can lead to depression, poor self-esteem, and a higher risk of injuries. These are unfortunately just a few of a much larger list of consequences.
The WHO estimates infections account for 31 percent of hearing loss cases. (Genetic and other causes account for 40 percent). Many infections that cause hearing loss can be prevented through vaccinations against such diseases as the mumps, measles, rubella, and meningitis. Although ear infections do not have a direct vaccine, the influenza shot can help in the prevention ear infections, another cause of hearing loss. Only 4 percent of childhood hearing loss is related to the use of ototoxic (toxic to the ear) medicines in expectant mothers and newborns.
To help prevent and care for childhood hearing loss, the WHO suggests these strategies: strengthen the child's immune system through vaccinations; implement better and more wide-spread early-intervention programs; train healthcare providers on how to better care for those with hearing loss; make hearing devices more readily accessible; push for legislation that regulates and restricts the sale of ototoxic medicines and environmental noise as well as implements standards for safe listening; and raise public awareness around the need for ear and hearing healthcare and programs worldwide.
Preventing hearing loss is a challenging task. However, there are already a few programs in action to help us out. In the U.S., thanks to Universal Newborn Hearing Screening legislation, which HHF was instrumental in establishing, 94 percent of newborns are tested for hearing loss before leaving the hospital, compared with just 5 percent in 1995! There are two tests that are currently available, both are reliable, and they can be used either separately or together. In the optoacoustic emissions test, a soft foam earphone and microphone are placed in the ear. The hearing specialist plays various sounds and measures the response. For the auditory brainstem response test, noninvasive electrodes are placed on the baby's head to detect auditory nerve responses to sounds the hearing specialist plays.
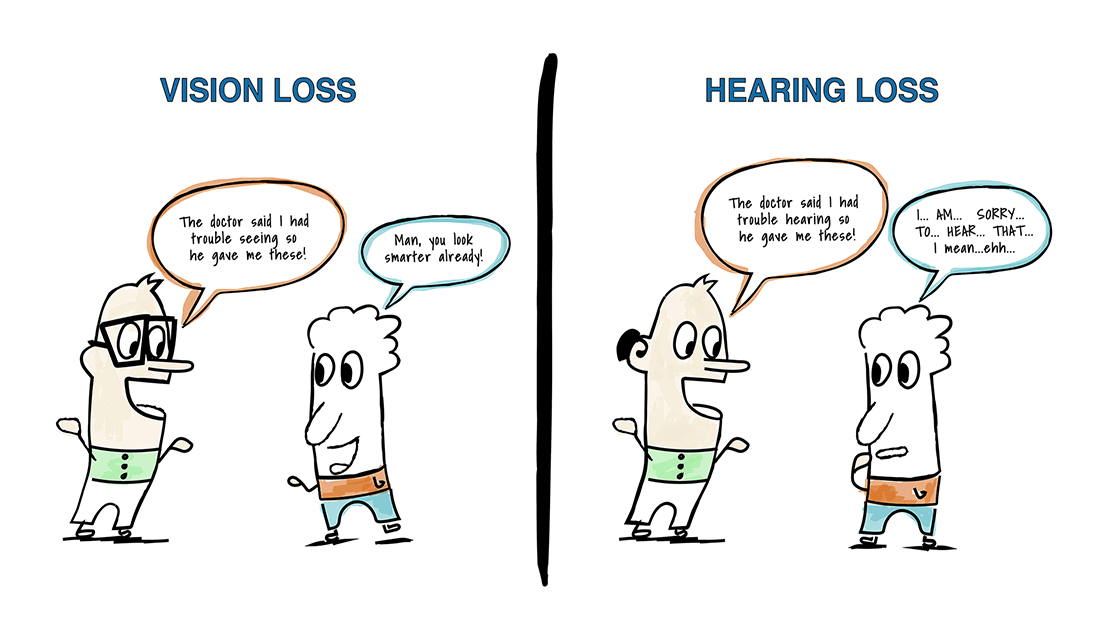
Hearing loss can be devastating for a child as well their family. Not being able to hear can affect all aspects of life, but learning how to prevent and to care for hearing loss can change a child’s life. In addition to the WHO’s “Childhood Hearing Loss: Act Now, Here’s How!”, here are HHF resources on children and hearing loss:
Ages and Stages: A speech-language pathologist discusses the process of verbal communication.
Tips for Hearing Well In the Classroom: Tips on how to work with a child’s teacher to implement a hearing regimen.
Visual Learning, Visual Teaching: Everything in life has a silver lining, even hearing loss.
"Listen to Me, Right Now!": What to do if your child doesn’t respond to repeated entreaties—especially when you’re not facing him or her.
New Beginnings: Advice from parents for parents for how to prepare for the 1st day of school when your child has hearing loss.
The Dangers of iPod Use: Answers to common questions about hearing protection for children and teens.