By Ian Swinburne, Ph.D.
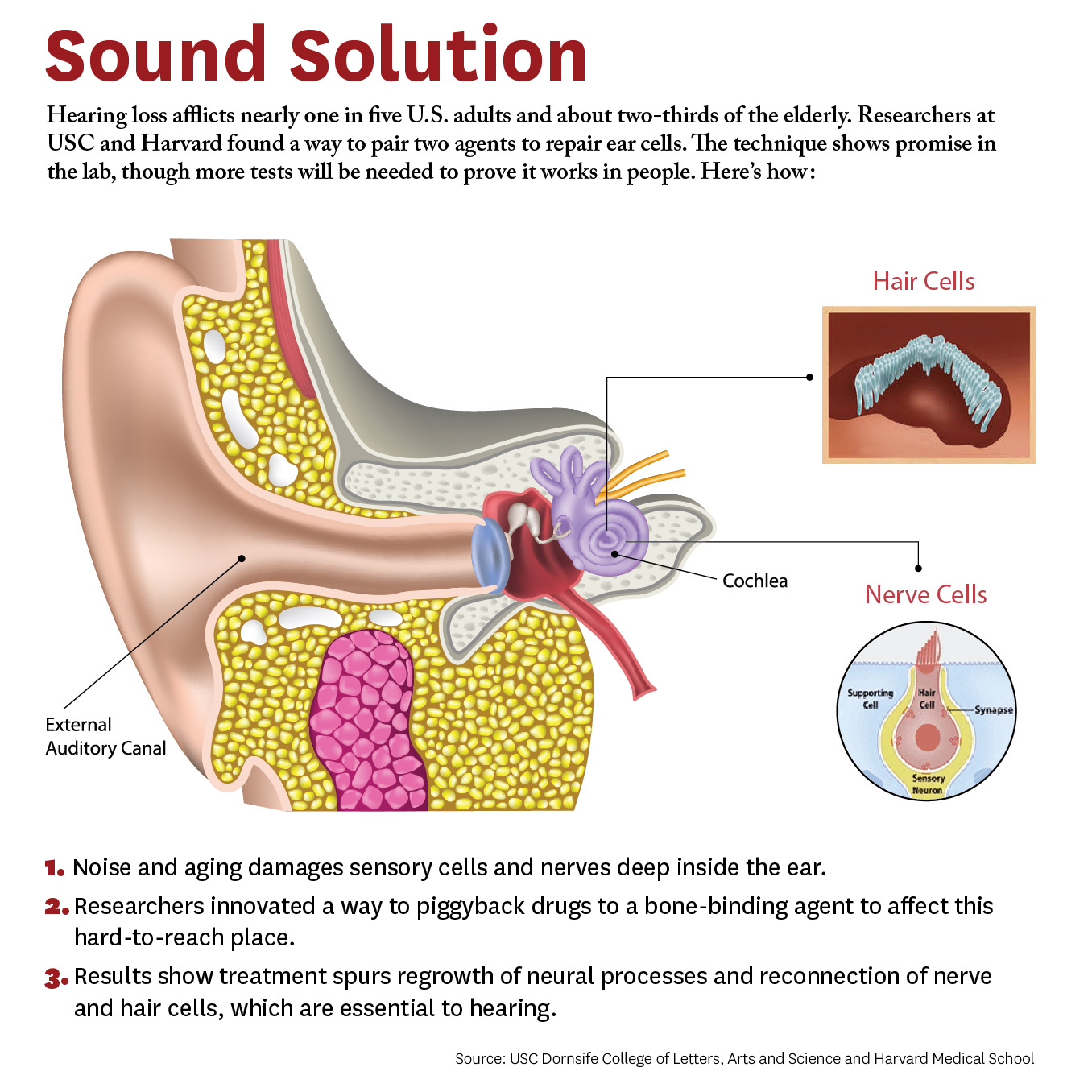
The inner ear senses sound to order to hear as well as sensing head movements in order to balance. Sounds or body movements create waves in the fluid within the ear. Specialized cells called hair cells, because of their thin hairlike projections, are submerged within this fluid. Hair cells bend in response to these waves, with channels that open in response to the bending. The makeup of the ear’s internal fluid is critical because as it flows through these channels its contents encode the information that becomes a biochemical and then a neural signal. The endolymphatic sac of the inner ear is thought to have important roles in stabilizing this fluid that is necessary for sensing sound and balance.
This study helps unravel how a valve in the inner ear's endolymphatic sac acts to relieve fluid pressure, one key to understanding disorders affected by pressure abnormalities such as Ménière’s disease.
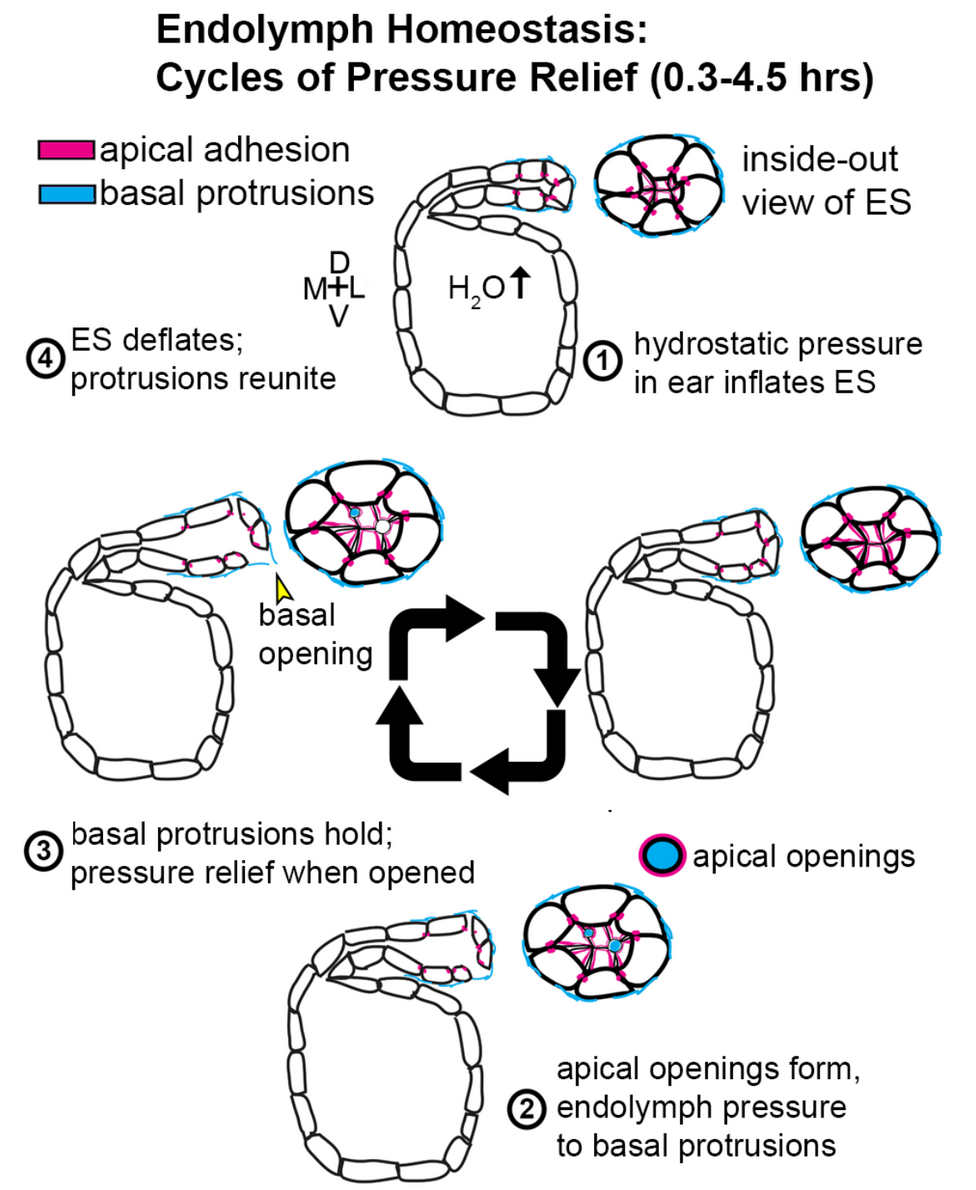
While imaging transparent zebrafish, my team and I found a pressure-sensitive relief valve in the endolymphatic sac that periodically opens to release excess fluid, thus preventing the tearing of tissue. In our paper published in the journal eLife June 19, 2018, we describe how the relief valve is composed of physical barriers that open in response to pressure. The barriers consist of cells adhering to one another and thin overlapping cell projections that are continuously remodeling and periodically separating in response to pressure.
The unexpected discovery of a physical relief valve in the ear emphasizes the need for further study into how organs control fluid pressure, volume, flow, and ion homeostasis (balance of ions) in development and disease. It suggests a new mechanism underlying several hearing and balance disorders characterized by pressure abnormalities, including Ménière’s disease.
Here is a time-lapse video of the endolymphatic sac, with the sac labeled “pressure relief valve” at 0:40.
2017 Ménière’s Disease Grants scientist Ian A. Swinburne, Ph.D., is conducting research at Harvard Medical School. He was also a 2013 Emerging Research Grants recipient.