By Rebecca M. Lewis, Au.D., Ph.D., and Jennifer Stone, Ph.D.
Mammals including humans cannot regenerate hair cells, but other species such as birds and fish readily regenerate hair cells after damage to restore auditory function. The gene ATOH1 produces a protein that pushes supporting cells—cells that neighbor hair cells—to either directly convert into a hair cell or to divide and form a new hair cell. However, ATOH1 expression (when the gene is turned on) does not guarantee that hair cells develop in birds or mammals, which suggests that there are factors that prevent supporting cells from changing into hair cells. Identifying these factors in birds may help us better understand the lack of hair cell regeneration in mammals.
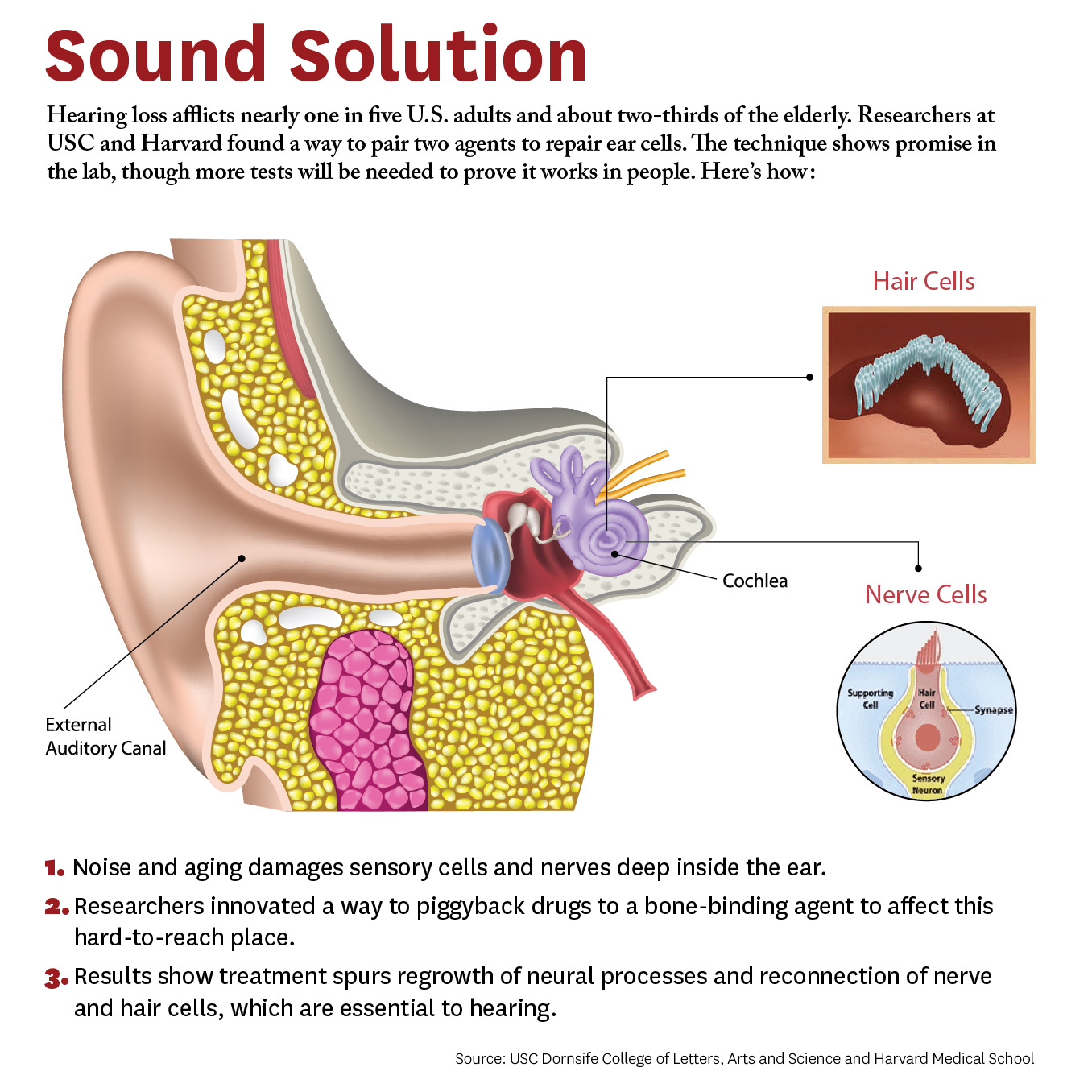
This schematic depicts our current ideas for how BMP4 regulates ATOH1 expression and therefore hair cell regeneration in the avian hearing organ. It shows (from left) typical hair cells, hair cell damage, and hair cell regeneration. Typical hair cells secrete BMP4. When hair cells die, BMP4 signaling is reduced, which allows ATOH1 to be expressed in supporting cells and pushes supporting cells to turn into hair cells. The newly regenerated hair cells secrete BMP4, suppressing ATOH1 in supporting cells and restoring the normal condition.
We examined the avian auditory system to characterize a potential inhibitor to ATOH1 during hair cell regeneration: bone morphogenetic protein 4 (BMP4). Bone morphogenetic proteins are secreted signaling molecules that regulate cellular processes in many regions of the body, including the nervous system. We found that BMP4 localizes to hair cells of the mature avian hearing organ and disappears when hair cells die or sustain damage. From this, we hypothesized that BMP4 may prevent ATOH1 expression in supporting cells and loss of BMP4 when hair cells die may enable ATOH1 to be expressed in supporting cells, driving them to convert into hair cells.
When we exposed avian auditory organs to BMP4 after selectively killing hair cells, this prevented ATOH1 expression and hair cell regeneration. When we antagonized BMP4 using an inhibitor, we found a generally opposite result: an increase in the number of regenerated hair cells.
We conclude that BMP4 is a potent inhibitor of ATOH1 and therefore suppresses hair cell regeneration. We recommend that BMP4 be explored further in studies of mammalian hair cell regeneration.
Published in Hearing Research on May 2, 2018, this study detailing BMP4’s negative effect on ATOH1 expands our knowledge of signaling molecules that suppress hair cell regeneration in birds and may also modulate hair cell regeneration in humans.
Rebecca M. Lewis, Au.D., Ph.D., is a clinical audiologist and auditory neuroscientist at Massachusetts Eye and Ear/Harvard Medical School in Boston. HRP researcher Jennifer Stone, Ph.D., is the director of research in the department of otolaryngology–head and neck surgery at the Virginia Merrill Bloedel Hearing Research Center at the University of Washington.
Empower the Hearing Restoration Project's life-changing research. If you are able, please make a contribution today.