Shelley Witt is a pioneering audiologist at the University of Iowa, one of the few who has recognized the differences between loudness hyperacusis and pain hyperacusis. Here, she discusses how she learned that the conventional wisdom is harmful to pain hyperacusis patients.
By Shelley Witt, M.A., CCC-A
(Este artículo también está disponible en español.)
While I was getting my undergraduate degree in psychology, I worked as a nanny for a deaf family. At the time I knew just enough basic sign language to get by.
This family was culturally Deaf and proud of it, so when they had a new child the baby announcement said: “Proud to announce a fourth-generation Deaf child.” This was back when cochlear implants were in their infancy.
I nannied for them for many years. I really liked the family and the experience, which opened up a new world for me.
Toward the end of my nanny days, a professor told me about a research position involving cochlear implants. In this position I was exposed to the other side of deafness: parents with typical hearing whose children were born deaf. I watched how many of these parents managed their child’s deafness, which was with grief.
I’ve enjoyed a variety of roles over the course of my 30-year audiology career, but about midway through I grew bored and desired a new and exciting challenge. I approached Richard Tyler, Ph.D., the director of the University of Iowa Tinnitus and Hyperacusis Clinic. He asked me, “Would you be interested in working with individuals with tinnitus and/or hyperacusis?” All I knew about hyperacusis was that it was sensitivity to sound. That was 16 or 17 years ago and there was little knowledge in this area.
I discovered that sound therapy could be helpful, and it was exciting because I saw people get better quickly. Starting by introducing simple ear-level devices with broadband noise at a very low volume, I could work patients up to near-typical sound tolerance levels very successfully. Even if it didn’t work, it didn’t make things worse, I reasoned, so in my mind it was a no-brainer.
I became cocky. This was the easiest thing in the world to treat! Why didn’t we learn about it in graduate school?
For a few years, I saw about 20 hyperacusis patients a year, treating them with sound therapy and getting great results. I kept five- to 10-year follow-up data on some of them, and they were doing great.
A Unique Type of Pain
Sound therapy worked—until it didn’t. For one patient, it quickly made the condition worse.
I thought, “Wait, she doesn’t have hyperacusis. I don’t know what she has.” Through this experience I learned that there can be differing severities, and that I had been treating individuals with loudness hyperacusis, who would report that sudden loud sounds—like clinking dishes, crying babies, and bursts of laughter—were bothersome, but not necessarily painful. Nor were they debilitating.
I learned that there were many individuals who wanted help but couldn’t even make it to the clinic. One patient had a family member call, explaining that the patient couldn't come see me, unable to handle the noise of the car ride.
Now, years later, I understand that pain hyperacusis is a completely different subcategory. People with loudness hyperacusis are bothered and might even feel pain, but it is not debilitating. They don’t have the same type of pain as individuals with pain hyperacusis, and they don’t have setbacks.
People with loudness hyperacusis even say things like, “When I go in the kitchen I just tough it out.” People with pain hyperacusis cannot tough it out. I realized that patients were self-selecting, meaning I was only seeing those who were well enough to travel to the clinic. In the spectrum of severity, their hyperacusis was mild, or moderate at worst.
Pain hyperacusis is different, and there is a unique type of pain associated with it. People call in from all over the world, and their description of the pain is eerily similar: a burning, stabbing, jabbing pain that feels like someone is pushing hot pokers into their ears. It is so very distinct.
Some patients with hyperacusis also have tinnitus. However, I do see individuals with loudness hyperacusis but no tinnitus. Unfortunately for some people, their hyperacusis is improved with sound therapy but they end up with ringing ears. Did we bring on tinnitus with sound therapy or would it have come on its own? There is still a lot we don't know.
So I’ve gone from a confident, cocky approach to a very cautious one. And I’m doing a lot of listening in trying to understand this ear disorder.
Another thing we don’t understand is the delayed reaction we see with pain hyperacusis. I consulted with a patient who had severe loudness hyperacusis. He was successfully treated with sound therapy, which allowed him to get out of the basement closet he had retreated to, and then out of the house and into the world.
However, he then started to report that, although he could manage many loud environmental sounds at the moment, a few days later he would experience severe delayed pain. This was a new symptom for me to try to understand. This patient did not regress back into the basement, but due to the severe delayed pain he had to resort to lifestyle modifications to manage sound outside of the house. I feel that we treated the loudness hyperacusis, but perhaps it morphed into pain hyperacusis.
Loudness discomfort levels (LDLs) are a measure often used by clinicians to assess the severity of hyperacusis. Patients are exposed to multiple tones or beeps at several different frequencies, and are asked to rate the loudness of the stimuli on a specific scale (i.e., very soft, soft, moderate, moderately loud, etc.) to determine at what level a sound becomes uncomfortably loud. I don’t appreciate this test measure.
It’s an unreliable test that can vary among clinicians simply based on the instructions used to complete the task. I also find that most people in pain are scared to do the LDL test, and I don’t blame them. I also worry that some individuals with delayed pain might end up being reinjured by an LDL test.
I have worked with enough loudness hyperacusis patients to see that sound therapy can be very effective. However, that is not the case with pain hyperacusis. I find that sound therapy can quickly make things worse, so I can only conclude that this must represent two very different hyperacusis subcategories.
A Spectrum Ear Disorder?
Is this a spectrum ear disorder? Could be.
Can loudness hyperacusis turn into pain hyperacusis due to various reasons such as an additional noise insult or an ototoxic drug? Maybe.
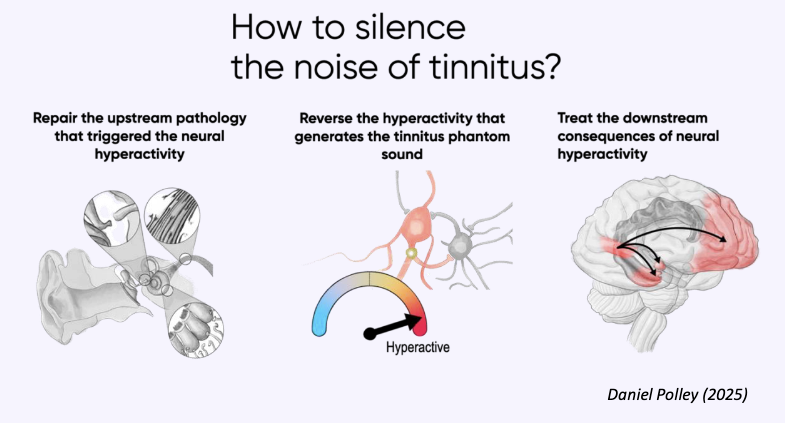
I feel that we need to start separating these two patient populations and studying them as having unique underlying pathologies that require very different treatment approaches.
The field of hyperacusis is still in its infancy. The information out there is that sound therapy is good and too much ear protection is bad. That information is harmful for patients with pain hyperacusis.
Pain hyperacusis patients are not overprotecting their ears. They are trying to survive. Sound is actually activating pain receptors, and it can cause catastrophic reactions. Without sufficient protection, they can readily worsen.
As an audiologist, I now know it’s wrong to tell pain hyperacusis patients to stop wearing earplugs or earmuffs or to initiate sound therapy.
So what’s left? Lifestyle modifications. Most of these people are already doing modifications because it’s the only way they can get through the day.
Such modifications generally include soundproofing at home, giving up typical kitchen dishes in favor of paper plates, and wearing ear protection for dangers like food packaging, etc. People with pain hyperacusis are often forced out of work because they simply cannot manage the sound environment of even a typical office. Something as ordinary as a ringing phone is a hazard.
What I can do, as the audiologist, is educate the people around them and help them understand that this is a real ear disorder. Pain hyperacusis can cause great destruction in relationships. People with healthy ears don't believe it, don’t understand it, and accuse sufferers of malingering. The truth is that this is not a psychological situation—it is a real pain condition.
Hyperacusis often starts with noise overexposure. Two people can be in the very same noise environment and one walks out unscathed while the other walks out with hearing loss, tinnitus, hyperacusis, or all three. Some ears are more susceptible than others, but susceptible to what and how we don’t know or understand yet.
With current research—most of it due to the heroic efforts of the late Bryan Pollard, who founded the nonprofit Hyperacusis Research—we are starting to make connections at a cellular level.
This is the most hopeful I have been in all the years I have been working with tinnitus and hyperacusis patients.
Right now, patients know how difficult it is to live with pain hyperacusis, and how much suffering it entails. Our immediate task is to increase awareness in the professional and clinical communities.
Shelley Witt, M.A., CCC-A, is a research audiologist at the University of Iowa. Hearing Health Foundation is grateful to have had a long, ongoing partnership with Hyperacusis Research, founded by the late Bryan Pollard, through which we fund the most promising hyperacusis investigations. Learn more at hhf.org/grants/hyperacusis.
This article is also available in Spanish.






Because noise-canceling earbuds are so comfortable and block everything out, people wear them for three, four, five hours straight without realizing the cumulative effect on their ears.