"In 2011, the Hearing Health Foundation based in New York, created the Hearing Restoration Project, a consortium of fourteen scientists who agreed to work together toward that goal, partly with funding from the foundation. One of the originators of the project, Edwin Rubel, who was a co-discoverer of hair-cell regrowth in chickens, told me, “It’s potentially the best thing that ever happened, because it really does bring together a lot of different kinds of expertise.”
Hearing Health Foundation's work toward finding better therapies and cures for hearing loss and tinnitus was featured in the April 3, 2017 Issue of T High-Tech Hope for the Hard of Hearing he New Yorker Magazine. Read the article here.
Our 2016 Annual Report Is Now Available!
By Frankie Huang
Hearing Health Foundation (HHF) is happy to announce that its 2016 annual report is now available. The report is an in-depth review of our activities, events, and achievements for fiscal year 2016. We are very proud of top marks from top charity-rating agencies and even more proud our audited financial statements.
We are fortunate to have such generous supporters who raised funds to further HHF’s mission of prevention, education, and research. Check out our supporters' creative and unique fundraisers; if you feel inspired and would like to organize an event of your own, please contact us at development@hhf.org.
In 2016, the Hearing Restoration Project (HRP) has made significant strides, bringing us closer to finding a cure for hearing loss and tinnitus. Here are just two of the HRP’s discoveries:
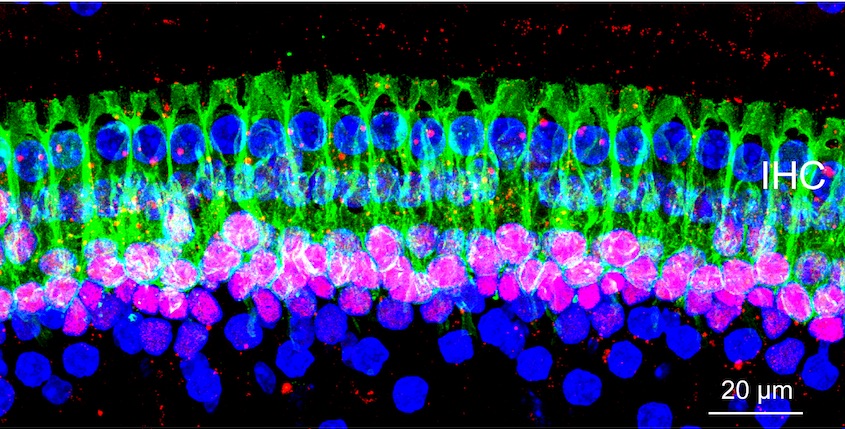
Successfully disrupted gene expression in the adult mouse cochlea, including capturing high-quality images—necessary for testing genes in regeneration.
Confirmed that the “DTR mouse” is an excellent platform for studying ways to stimulate hair cell regeneration in the mammalian inner ear.
HHF awarded nine Emerging Research Grants (ERGs) to early-career scientists who are pursuing projects in the areas of Central Auditory Processing Disorder (CAPD), Hyperacusis, Ménière's disease, Stria, and Tinnitus. Through ERG, we hope to uncover better treatment options and deeper understanding of these disorders.
Last but certainly not least, we want to express our gratitude and appreciation for our many donors; because of their support, we were able to continue with our important work. To see your name on our next donors’ list, we gladly welcome and appreciate your gift in any amount made by Sept. 30, 2017.
Urgent Call to Action: Proposed Cuts to Hearing Research
By Nadine Dehgan, Elizabeth Keithley, Ph.D., and Peter Barr-Gillespie, Ph.D.
Hearing Health Foundation (HHF) is deeply concerned to learn the Trump administration has proposed an 18% cut to the budget for the National Institutes of Health (NIH).
Such a cut would be devastating for all medical research - including hearing research. As an advocate for the millions of Americans who have hearing loss we are especially troubled.
A drastic decrease to the funding of hearing research would disrupt the efforts of the many hearing researchers who dedicate their lives to finding cures and treatments for hearing loss, tinnitus and balance disorders.
HHF and the NIH are partners in funding research. HHF’s two research programs—the Emerging Research Grants and the Hearing Restoration Project—both rely on NIH support. HHF's funding alone cannot support these labs.
Private funding of hearing research is dwarfed by NIH support, and these proposed cuts could harm the research program of each and every hearing research lab, including those supported by the HHF.
As people with hearing loss, parents of those with hearing loss, children of those with hearing loss and as the leadership of the Hearing Health Foundation we ask your support. Financial support is always needed and welcome - but in this case we are specifically asking for you to contact your representatives to let them know that you oppose cuts to the NIH (and in fact support increases to the NIH’s budget).
If you are passionate about funding the research that will lead to cures for hearing loss and balance disorders, now is the time to act.
Please join us in contacting your Senators and House Representative's offices today.
With our sincere thanks,
Nadine Dehgan | CEO of HHF
Elizabeth Keithley | Chair of the Board
Peter Barr-Gillespie | HRP Scientific Director
Low Income at Disproportionate Risk for Hearing Loss
By Morgan Leppla
Hearing loss affects people of every age, race, and socioeconomic level. However, there are circumstances that put different people in danger of acquiring it. While some causes of hearing loss are avoidable or controllable, others are are not easily escaped. Low income people are much more likely to suffer from hearing loss than those who earn higher salaries, witnessed in both children and adults.
There are a number of reasons for this disproportional risk. Access to regular and preventative health care can be scarce so the prevalence of health problems tends to be higher overall, including that of hearing loss. Middle ear infections are more common, as is lead poisoning and malnutrition. Such detriments affect physical as well as mental development in children, and impact socio-emotional and academic performance. This disparity is heightened within underfunded school systems where sufficient accommodations for all disabilities, including hearing loss, may not be available.
Low income caretakers of children experience additional external burdens due to a host of factors, such as long work schedules, literacy level, and language proficiency. These factors also make it difficult for caretakers to advocate on behalf of their children, or possibly notice their children’s developmental delays as a result of potential hearing loss.
Low income individuals who have emigrated from developing nations are also more likely to have already experienced some degree of permanent hearing damage. They are also often ushered into low-paying jobs that can include occupational workplace hazards like dangerously loud noises or exposure to chemicals.
People of color have a higher risk for acquiring hearing loss. While non-Hispanic Whites still constitute the largest single group of Americans living in poverty, ethnic minority groups are overrepresented (27.4 percent African-American; 28.4 percent American Indian and Alaskan Native; 26.6 percent Hispanic, and 12.1 percent Asian and Pacific Islander compared with 9.9 percent non-Hispanic White).
Lastly, men of all races, in low income jobs that may include physical labor, are even more at risk than other men. (If you didn’t already know, men are more likely than women to have a hearing loss, regardless of income levels).
Preventing hearing loss requires effort communicating with groups that are more at risk. If we are to end hearing loss as an epidemic, it makes sense to promote and extend hearing health care to populations who could use it most.
Under Normal Circumstances
By Morgan Leppla
March is Disability Awareness Month. In honor of this important awareness month, Hearing Health Foundation is raising awareness and celebrating all of our different abilities and doing our part to reduce the stigma of living with hearing loss and its associated disorders.
Whether we like it or not, people compare themselves to others. Maybe contemporary culture brings it out in us, or perhaps that impulse is rooted in Darwinism ideology of survival of the fittest, reminding us of competitive advantages. Who is taller, more intelligent, faster?
Possibly, it also has to do with how we conceptualize normalcy. In the mid-1800s, Belgian statistician Adolphe Quetelet introduced the idea of “l’homme moyen” (average man) when he realized that human traits are distributed over a bell curve. So the average man would have the mean of all human traits in a single abstract person.
“Normal” entered English vocabulary in 1840 and has since been used to describe bodies and behavior. However, before society focused on the “the norm” it concerned itself with “the ideal.” Take the most coveted parts of bodies and traits that exist and combine them, and that would be the ideal person.
So why is this distinction meaningful? Because every living person is non-ideal, since by definition it cannot exist in one person, whereas people (bodies and traits) can be “normal.” On the contrary, normalcy is attainable on an individual level. And society’s reactive effect to the creation of normal humans was the production of their dichotomous counterparts: the extremes or deviants at the tail ends of the bell curve, the abnormal.
However, a collision of the normal and the ideal occurred when English statistician Francis Galton decided to rank human traits, created quartiles on an intelligence bell curve, and ordered them one to four. One was lowest intelligence and least desirable while four was highest intelligence and most desirable. He reoriented the human ideal using the norm. And now, I would say, it is “normal” to want to be the smartest, most athletic, most attractive, etc.?
The latter half of the 19th century employed pseudo-empirical justifications for describing how bodies should be in fairly clear terms. And to focus on distribution of differences warps the way society approaches normalcy as a concept. It allows us to draw lines where perhaps they ought not exist.
Thus we arrive at the construction of disability. Anyone who does not physically look like others or does not act like others is perceived as deviant or abnormal because they are at the wrong end of the bell curve. Beyond the initial construction of the human normal, barriers that are literal, educational, communicational, and attitudinal further maintain “disability” since nonexistent or poor accommodations along with stigma exacerbate “disabling” differences.
Hearing Health Foundation is encouraging everyone to think about how “norms” have molded our preferences and attitudes and whether that translates to treating people differently. Life may be more arbitrary than you think, and more can be going on than what meets the eye.
HHF is committed to spreading awareness of hearing loss and its associated disorders as well as reducing the stigma attached to them. If you’d like to share your story and experiences with our community, please email us at info@hhf.org.
Make a Sound Investment
By Frankie Huang
In honor of World Hearing Day, which takes place on March 3 every year, Hearing Health Foundation is joining forces with the World Health Organization (WHO) to draw attention to the economic impact of hearing loss and the importance of treating hearing loss.
Did you know the economic cost for unaddressed hearing loss is estimated to be $750 billion globally? In the U.S. individuals with untreated severe to profound hearing loss are expected to cost society $270,000 each over the course of their lifetimes. Most of these costs are due to reduced productivity in the workplace, although the use of special education resources among children and other social services are also factors.
Lifetime earnings for those with untreated hearing loss average 50 to 70% less than their typical-hearing peers in the U.S., and has been shown to negatively impact household income up to $12,000 per year, on average, depending on the degree of hearing loss, according to the Better Hearing Institute. This is largely due to having fewer opportunities for promotions, reduced job performance, and decreased earning power.
Beyond economic losses, untreated hearing loss can significantly impact a person’s quality of life. Researchers have found that individuals with untreated hearing loss are more likely to develop depression, anxiety, and feelings of inadequacy. They may also avoid or withdraw from social situations. Left undetected in children, hearing loss can negatively impact speech and language acquisition, academic achievement, and social and emotional development.
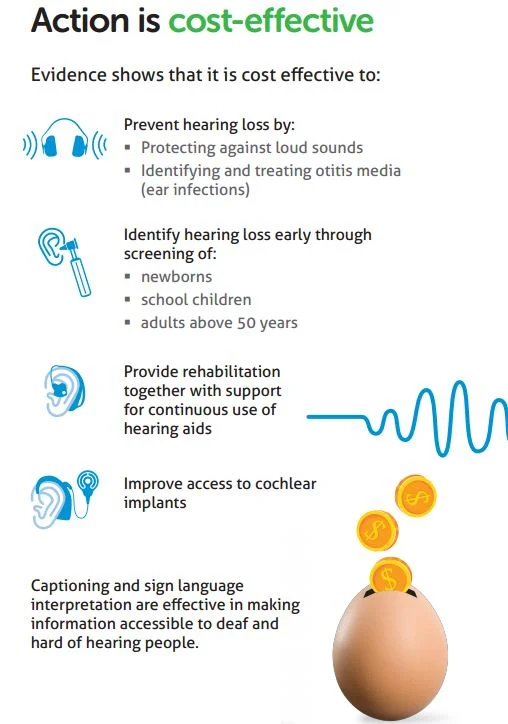
Prevention, screening for early identification, early intervention, and rehabilitation through hearing devices are among the strategies that mitigate hearing loss and its consequences. Those who treat their hearing loss with hearing aids and/or cochlear implants show improvement in social, emotional, and psychological well-being. Interventions can significantly decrease isolation, increase self-esteem, and lead to better employment opportunities and earnings—all of which will benefit society as a whole.
For World Hearing Day 2017, the WHO has joined forces with Mimi Hearing Technologies. To raise awareness of hearing loss, Mimi hopes to have 1 million people test their hearing. To do this, they are offering the Hearing Test app on iOS free for everyone. If you suspect you or a loved one may have hearing loss, this is a great opportunity to test your hearing with Mimi’s Hearing Test, which is an initial online assessment. The results may require a follow-up appointment with a hearing health professional. However, by detecting signs of hearing loss early on the benefits of treating hearing loss far outweigh the consequences if left untreated.
Second Cause of Hidden Hearing Loss Identified
By Michigan Medicine - University of Michigan
Some people can pass a hearing test but have trouble understanding speech in a noisy environment. New research identifies a new mechanism for this condition just years after its discovery. Credit: Michigan Medicine
Patients who complain they can't hear their friends at a noisy restaurant, but pass a hearing test in their doctor's office, may be describing hidden hearing loss.
Now, less than six years since its initial description, scientists have made great strides in understanding what hidden hearing loss is and what causes it. In research published in Nature Communications, University of Michigan researchers report a new unexpected cause for this auditory neuropathy, a step toward the eventual work to identify treatments.
"If people can have hidden hearing loss for different reasons, having the ability to make the right diagnosis of the pathogenesis will be critical," says author Gabriel Corfas, Ph.D., director of the Kresge Hearing Research Institute at Michigan Medicine's Department of Otolaryngology -- Head and Neck Surgery.
Corfas published the research with co-author Guoqiang Wan, now with Nanjing University in China. They discovered using mice that disruption in the Schwann cells that make myelin, which insulates the neuronal axons in the ear, leads to hidden hearing loss. This means hidden hearing loss could be behind auditory deficits seen in acute demyelinating disorders such as Guillain-Barré syndrome, which can be caused by Zika virus.
Corfas and Wan used genetic tools to induce loss of myelin in the auditory nerve of mice, modeling Guillain-Barré. Although the myelin regenerated in a few weeks, the mice developed a permanent hidden hearing loss. Even after the myelin regenerated, damage to a nerve structure called the heminode remained.
Synapse loss versus myelin disruption
When the ear is exposed to loud noises over time, synapses connecting hair cells with the neurons in the inner ear are lost. This loss of synapses has previously been shown as a mechanism leading to hidden hearing loss.
In an audiologist's quiet testing room, only a few synapses are needed to pick up sounds. But in a noisy environment, the ear must activate specific synapses. If they aren't all there, it's difficult for people to make sense of the noise or words around them. That is hidden hearing loss, Corfas says.
"Exposure to noise is increasing in our society, and children are exposing themselves to high levels of noise very early in life," Corfas says. "It's clear that being exposed to high levels of sound might contribute to increases in hidden hearing loss."
The newly identified cause -- deficiency in Schwann cells -- could occur in individuals who have already had noise exposure-driven hidden hearing loss as well. "Both forms of hidden hearing loss, noise exposure and loss of myelin, can occur in the same individual for an additive effect," Corfas says.
Previously, Corfas' group succeeded in regenerating synapses in mice with hidden hearing loss, providing a path to explore for potential treatment.
While continuing this work, Corfas started to investigate other cells in the ear, which led to uncovering the new mechanism.
There are no current treatments for hidden hearing loss. But as understanding of the condition improves, the goal is for the research to lead to the development of drugs to treat it.
"Our findings should influence the way hidden hearing loss is diagnosed and drive the future of clinical trials searching for a treatment," Corfas says. "The first step is to know whether a person's hidden hearing loss is due to synapse loss or myelin/heminode damage."
Materials provided by Michigan Medicine - University of Michigan. Co-author Guoqiang Wan, Ph.D., was a 2014 Emerging Research Grants recipient funded by the Wes Bradley, M.D. Memorial Grant.
We need your help in funding the exciting work of hearing and balance scientists.
To donate today to support HHF's groundbreaking research, please visit hhf.org/donate.
Celebrating Hearing Innovations
By Frankie Huang
On Feb. 25, Hearing Health Foundation is celebrating International Cochlear Implant Day to raise awareness of this life-changing technology. Cochlear implants greatly enhance the lives of individuals with severe to profound hearing loss and individuals who don’t benefit from the use of hearing aids. Did you know that as of November 2012, there are 324,000 cochlear implants in use worldwide, and that number is growing daily!
Cochlear implants (CI) are electronic medical devices that are implanted via a surgical procedure. Although implants replace the function of the damaged inner ear, it is important to remember that CIs do not restore normal hearing but work by bypassing damaged structures in the inner ear and stimulating the auditory nerve. This sends signals to the brain, allowing the user to perceive sounds.
Researchers found that children 5 years or older with bilateral severe or profound hearing loss who are implanted with CIs have better speech perception and development over time than children treated with hearing aids. In addition, children with profound hearing loss who used CIs showed greater development of preverbal behavior than those using hearing aids.
Other researchers found that children receiving CIs before 24 months of age greatly benefit in terms of their overall language development. Levels of spoken language in children implanted before age 24 months were on par with their typical hearing peers by age 4.5, but those implanted after age 24 months did not “catch up” with hearing peers by age 4.5. It’s important to note the study didn’t evaluate language development or ongoing delays after age 4.5.
HHF is proud to have supported research in the 1970s that led to the development of cochlear implants. Since then the technology has continued to evolve and improve in order to increase the benefits yielded from having a cochlear implant and to reduce risks associated with an invasive surgical procedure. By further improving the design and the function of CIs, researchers may find a way to maximize all the possible benefits for the patient, to preserve residual hearing, and to improve the health of the inner ear.
If you’re interested in funding research related to hearing loss technology,
please consider donating today at hhf.org/donate or contact us at development@hhf.org.
Presbycusis and the Deterioration of Neural Nets
Using two different mouse models, we show that PNN expression is reduced with age, and that an age-related decline in PNNs with presbycusis may be related to changes in synapse function, affecting the processing of sound, particularly those that require proper timing.
A Healthy Heart Could Mean Better Hearing Health
By Frankie Huang
In honor of American Heart Month in February, Hearing Health Foundation wants to shine light on the link between heart disease and hearing loss. According to the Centers for Disease Control and Prevention, 610,000 Americans die from heart disease each year, making it the leading cause of death for men and women in the U.S.
Heart disease is linked to or causes numerous health issues, including hearing loss. One study suggests that low-frequency hearing loss may be able to predict cardiovascular health. Using an audiogram, researchers were able to determine the probability of cardiovascular disease in men and women. The study found that there was a correlation of heart attacks in men, and a correlation of claudication (pain caused by too little blood flow) in women.
High blood pressure can also be a contributing factor to developing hearing loss, since the inner ear is sensitive to blood flow. High blood pressure damages blood vessels and increases the risk of plaque buildup in the arteries, making it harder for blood to flow throughout the body. In other words, inadequate blood flow and nerve damage in the inner ear may lead to irreversible hearing loss.
A common cause of heart disease and hearing loss is smoking. Smoking increases blood pressure and plaque buildup, and causes hardening of the arteries, all of which decreases blood flow to the organs and other parts of the body. The effects of smoking damages the cardiovascular system, boosting the risk of hearing loss. Additionally, cigarettes contains nicotine, disrupting the neurotransmitters in the auditory nerve (which tell the brain which sound you are hearing) and preventing the brain to accurately interpret sound. Cigarette smoke contains many harmful chemicals that are believed to be ototoxic (toxic to the ear) that may damage hair cells.
There are a variety of ways to prevent heart disease and cut your risk for hearing loss. Eating healthy and incorporating moderate exercise into your daily life can drastically improve your health. Include more fish in your diet: Salmon, mackerel, and herring are high in the omega-3 fatty acids that help reduce high blood pressure and prevent plaque buildup, so you can decrease your overall risk of hearing loss.