And what to do in response.
By Bruce L. Douglas, DDS, MPH
I am 98 years old this year and work at the University of Illinois School of Public Health, where I am a professor of health and aging. It is actually my sixth appointment at the university. I have been leading a research project on “the effect of senescence on the quality of life of older people,” with a high priority on communication ability, especially hearing loss.
This subject is near and dear to my heart. It’s of great concern to me that hearing problems do not receive their fair share of attention as research proceeds on issues of quality of life among the aging population.
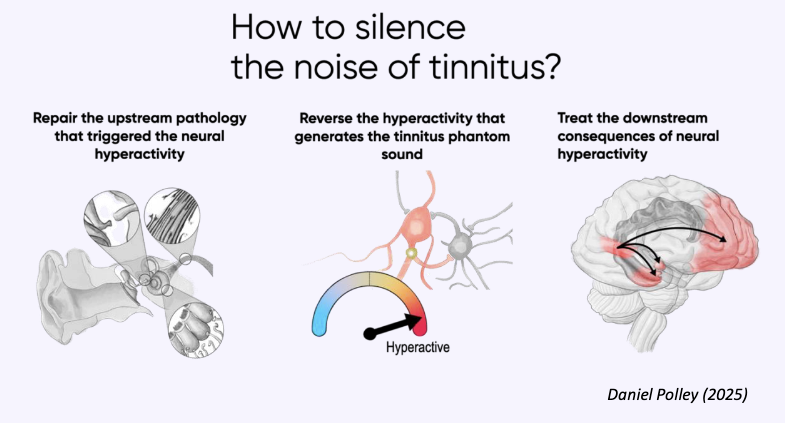
In addition to working as an oral surgeon, dentist, state legislator, and activist, I am a U.S. Navy veteran, and it was during my service, while on active duty during the Korean War, that a one-time noise exposure from an M1 rifle during a training exercise (none of us used hearing protection) left me with permanent, chronic tinnitus. I had earlier been living with a hearing loss, something my father and grandfather also experienced, although I did not use hearing aids till well after my service. After wearing hearing aids for decades, I had cochlear implant surgery in my right ear at age 91.
Even with this remarkable technology that continues to improve, managing our expectations of how well these devices do or do not work affects our ability to communicate. Here I detail the ups and downs.
Ups
Dr. Douglas with his wife Jan.
It’s no secret that there are lots of sounds that are better not heard, so on some occasions I actually turn off my hearing aids. I even do it at home when some voices are, in my opinion, better not heard by me! Of course, no one knows that I’ve escaped into the peaceful world of silence.
Since my hearing aid and cochlear implant are controllable on my cell phone, my wife, daughter, and grandson—all occupants of my home and with whom I eat dinner regularly—assume that I am being momentarily rude and answering a text message. Also, I can turn the sound down considerably if I wish, which is a unique characteristic of hearing assistive devices, as compared with human hearing capability.
Then, there’s the delightful experience of succumbing to deafness when I retire for the night, and my hearing devices are comfortably sitting in their dehydration machine. If you’re wondering how I handle emergencies, I have a device that flashes strobe signals if the burglar or fire alarm sounds off, and a vibrating pad under my pillow that I use to awaken in the morning. If my wife needs to communicate with me during the night, she has a button that turns on our bed lights and I have learned to read her lips if she wishes to tell me something important. My hearing aids are just an arm’s length away and available if necessary.
These ups are not gimmicks! My hearing devices are important parts of my life and my close relatives know and respect that fact.
Downs
Now to the “downs,” and there are many. Being hard of hearing, even with my advanced equipment at work in both ears, can be a drag! I have learned to live with most inconveniences that accompany near deafness, but doing so can, to put it mildly, be overwhelmingly tiring.
The tiredness that I feel at the end of a normal day at the university is unlike the tiredness one feels after working out or climbing flights of stairs. It is instead what I call cognitive exhaustion. It’s a sensation that can only be modified with one glass, in my case, of red wine, and 15 minutes of watching the TV news before I’m ready to rejoin the human race and sit down at the dinner table.
The hardest part of being hard of hearing is that you are a victim of an invisible condition. Therefore, companions or even knowledgeable close relatives either don’t know, or forget, that you have difficulty hearing, unless the environment around you has been modified to accommodate your hearing loss.
That’s not difficult to do at home, but it’s near impossible to do in the outside world. Most of us think of that world as “hostile” and the people in it “insensitive,” but it’s something to which we must adjust, if we want to remain working in parts of it.
We don’t want sympathy. We want sensitivity to the fact that we cannot communicate with someone effectively unless we can see that person’s mouth as they speak and the person with whom we are talking is “nearby”—meaning, in the same room.
Most of us hear the spoken word, but we have difficulty understanding it if it isn’t spoken clearly or spoken too rapidly. We invariably have difficulty with accents and high pitched sounds, which usually means women’s voices. Unfortunately most people with hearing loss are hesitant to spend a few moments explaining to their companion(s), at the beginning of a social interchange, that they are hard of hearing and that it would be very helpful if others would take that into account.
The Biggest Challenge
The sad reality is that such hesitancy often leads to the biggest problem in the arena of hearing loss, and that is people who are hard of hearing too frequently acting like they are hearing when the opposite is the case.
And they in effect deceive their companions into thinking that they are in on the conversation. In frustration, the person with a hearing loss uses facial expressions and head movements to lead their companion to assume that they are hearing and digesting everything that is being said. Depending on the nature of the relationship, the results of such deception on the part of the person with a severe hearing loss can cause social chaos and extreme embarrassment.
The personality of the person with a hearing loss relates intimately to how they act and react to adverse social situations. My advice is to follow the principles of prevention, which I break down into primary, secondary, tertiary, and auxiliary categories.
Primary prevention suggests that it may be wise to avoid these situations entirely. But if Covid has taught us anything it is that humans are social creatures, so completely avoiding social situations will not benefit our mental health.
Secondary prevention consists of prepping your audience beforehand about your problem. Request that when they are addressing you, they face you and try to speak slowly and clearly. At least you are informing people of your problem, and sparing yourself the social ostracization that sometimes accompanies such situations.
Auxiliary prevention consists of setting up the environment beforehand and taking into account the potential challenges. We can change the location of chairs, close curtains or drapes, turn off background music, and ask to chat in a location far from other competing conversations. We can delay communication until these parameters are met and/or we can talk face to face.
Personality, Age, and Advice
The personality and, usually, age of the person with a hearing loss are inextricably related to how well they can handle the “downs” of hearing loss. Let’s face it, it’s a tough life for people with hearing loss. We have to adjust to an unintentionally adverse world in which very few people have the patience and sensitivity to accept our handicap with equanimity.
It is not uncommon for those with hearing loss to compensate for not being able to hear in social situations to become the dominant speaker. I gradually realized, supported by my wife’s observations, that my tendency to lead or even monopolize discussions was that as long as I was talking, I did not have to strain to understand what other people were saying.
It is wise for those among us who find that withdrawal from social challenges is their last resort, to seek help from a therapist, preferably one who also has a hearing loss and understands the challenges from personal experience. That recommendation applies to people of all ages. It just isn’t worth the pain that results from withdrawal and the loneliness that accompanies it.
I believe the main way in which to approach the downs of hearing loss is to look in the mirror and decide, along with your closest friends and relatives, what you want (and need) out of life. Hearing aids and cochlear implants have improved tremendously in recent years, but they are still only devices to help you to subsist, under the best of circumstances, within your own capabilities and circumstances, in environments of your own choosing.
Groups, restaurants, large family gatherings, and any places with loud background noise are not places of comfort for those who have hearing loss and who want to participate in the activities that take place in such settings. Auxiliary prevention answers the question of how to handle mildly adverse environments, but it requires a degree of aggressiveness that is not within the comfort range of many people with hearing loss.
Finally, if I may speak for all of us with a hearing condition, I ask our family, friends, and folks we interact with on an everyday basis to please be patient. We have an invisible condition, most often beyond our control, and it’s all we can do to try to hear and listen to you and respond to the best of our ability.
Bruce L. Douglas, DDS, MPH, is a professor of health and aging at the University of Illinois at Chicago School of Public Health. He shared his hearing loss journey in the Fall 2018 issue of Hearing Health.






Because noise-canceling earbuds are so comfortable and block everything out, people wear them for three, four, five hours straight without realizing the cumulative effect on their ears.