Scientists from the University of Southern California (USC) Stem Cell laboratory of Neil Segil, Ph.D., have identified a natural barrier to the regeneration of the inner ear’s sensory cells, which are lost in hearing and balance disorders. Overcoming this barrier may be a first step in returning inner ear cells to a newborn-like state that’s primed for regeneration, as described in a study published in Developmental Cell in July 2021.
“Permanent hearing loss affects more than 60 percent of the population who reach retirement age,” says Segil, who is a professor in the department of stem cell biology and regenerative medicine, and the USC Tina and Rick Caruso department of otolaryngology–head and neck surgery. “Our study suggests new gene engineering approaches that could be used to channel some of the same regenerative capability present in embryonic inner ear cells.”
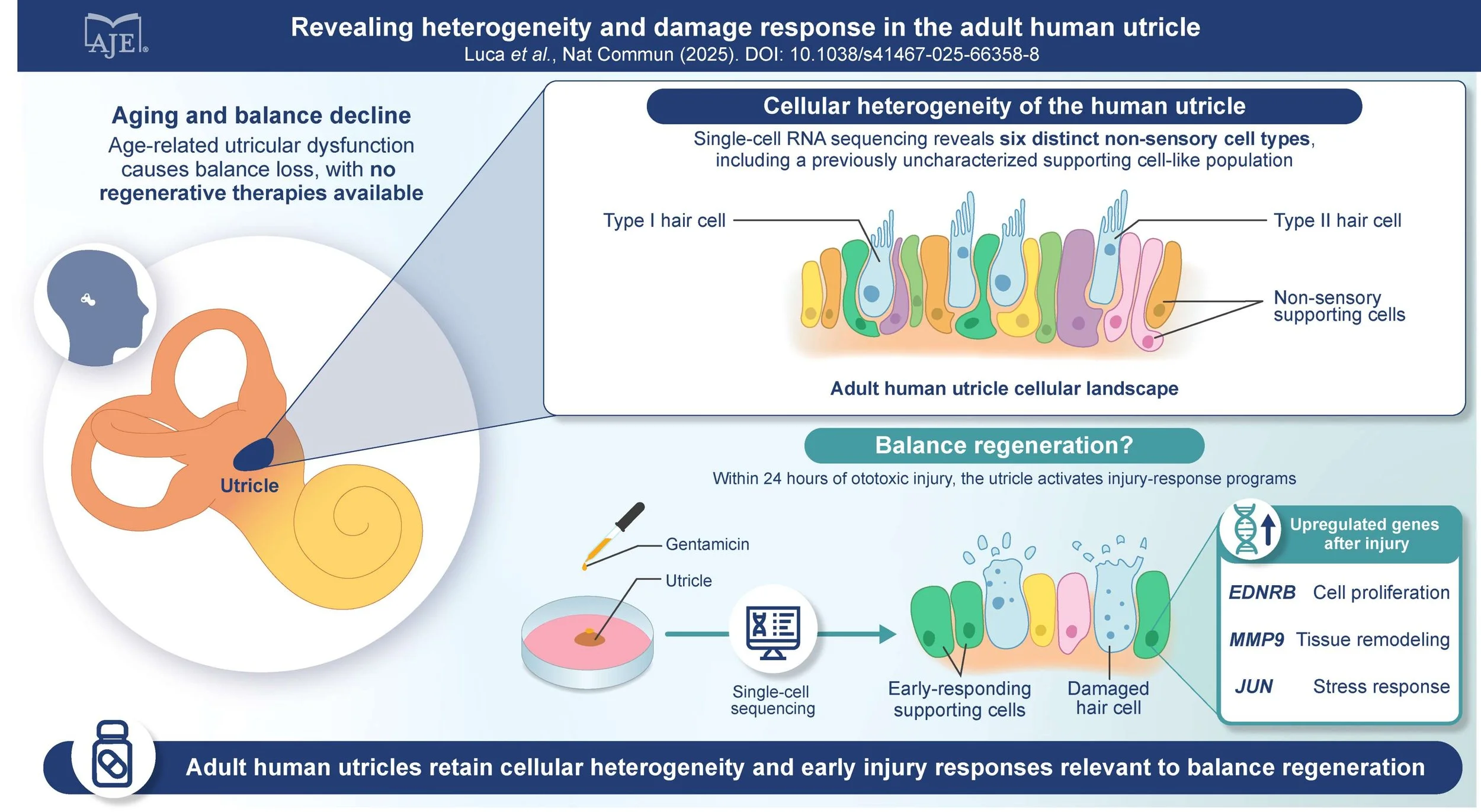
In the inner ear, the cochlea contains two major types of sensory cells: hair cells that have hairlike cellular projections that receive sound vibrations; and so-called supporting cells that play important structural and functional roles.
When the delicate hair cells incur damage from loud noises, certain prescription drugs, or other harmful agents, the resulting hearing loss is permanent in older mammals. However, for the first few days of life, lab mice retain an ability for supporting cells to transform into hair cells through a process known as transdifferentiation, allowing recovery from hearing loss. By age 1 week, mice lose this regenerative capacity—also lost in humans, probably before birth.
The organ of Corti, the hearing organ of the inner ear (cochlea), contains rows of sensory hearing cells (green) surrounded by supporting cells (blue). Photo by Yassan Abdolazimi/Segil Lab/USC Stem Cell
Based on these observations, postdoctoral scholar Litao Tao, Ph.D., graduate student Haoze (Vincent) Yu, and colleagues took a closer look at neonatal changes that cause supporting cells to lose their potential for transdifferentiation.
In supporting cells, the hundreds of genes that instruct transdifferentiation into hair cells are normally turned off. To turn genes on and off, the body relies on activating and repressive molecules that “decorate” the proteins known as histones. In response to these decorations known as epigenetic modifications, the histone proteins wrap the DNA into each cell nucleus, controlling which genes are turned on by being loosely wrapped and accessible, and which are turned off by being tightly wrapped and inaccessible. In this way, epigenetic modifications regulate gene activity and control the emergent properties of the genome.
In the supporting cells of the newborn mouse cochlea, the scientists found that hair cell genes were suppressed by both the lack of an activating molecule, H3K27ac, and the presence of the repressive molecule, H3K27me3. However, at the same time, in the newborn mouse supporting cells, the hair cell genes were kept “primed” to activate by the presence of yet a different histone decoration, H3K4me1. During transdifferentiation of a supporting cell to a hair cell, the presence of H3K4me1 is crucial to activate the correct genes for hair cell development.
Unfortunately with age, the supporting cells of the cochlea gradually lost H3K4me1, causing them to exit the primed state. However, if the scientists added a drug to prevent the loss of H3K4me1, the supporting cells remained temporarily primed for transdifferentiation. Likewise, supporting cells from the vestibular system, which naturally maintained H3K4me1, were still primed for transdifferentiation into adulthood.
“Our study raises the possibility of using therapeutic drugs, gene editing, or other strategies to make epigenetic modifications that tap into the latent regenerative capacity of inner ear cells as a way to restore hearing,” Segil says. “Similar epigenetic modifications may also prove useful in other non-regenerating tissues, such as the retina, kidney, lung, and heart.”
Along with Segil’s USC Stem Cell Lab, coauthors include Andy Groves, Ph.D., of Baylor College of Medicine and a fellow member of the Hearing Restoration Project at Hearing Health Foundation.
This is adapted from a USC press release. Neil Segil, Ph.D., a member of Hearing Health Foundation’s Hearing Restoration Project (HRP), is a professor in the University of Southern California’s department of stem cell biology and regenerative medicine and the USC Tina and Rick Caruso department of otolaryngology–head and neck surgery. Coauthor and fellow HRP member Andy Groves, Ph.D., is a professor and the Vivian L. Smith Endowed Chair in Neuroscience at Baylor College of Medicine, Texas. Coauthor Zlatka Stojanova, Ph.D., in the Segil Lab at USC, is a 2011–2012 Emerging Research Grants recipient.






These findings suggest that the ability to integrate what is seen with what is heard becomes increasingly important with age, especially for cochlear implant users.