(Desplácese hacia abajo para ver una traducción al español de este artículo.)
By Francisco Barros-Becker, Ph.D.
Mechanosensory hair cells play a pivotal role during balance and hearing. Unfortunately, many types of insult, like exposure to loud noises or certain therapeutic drugs, can cause permanent hearing loss by irreversibly damaging or killing these cells.
The class of aminoglycoside antibiotics are the standard of care for many serious bacterial infections. Studies report that hearing loss (a side effect known as ototoxicity) from undergoing these treatments can range from 11 to 67 percent.
Understanding how these drugs are able to kill hair cells may provide new potential therapeutic avenues to make these important drugs safer.
In our publication published in Frontiers in Neurology in November 2024, we explore how different aminoglycosides, like neomycin and gentamicin (or its chemical analog G418), are able to kill hair cells in distinctive ways. Using the zebrafish model, we observed that neomycin can kill hair cells in an acute way, with most of them gone within the first hour after exposure to the drug.
On the other hand, gentamicin or G418 kills in a delayed way, needing up to 24 hours to generate a comparable amount of hair cell death.
One of the previously seen hallmarks of a neomycin-driven hair cell death is the rapid, spike-like mitochondrial calcium uptake preceding the death of the hair cell. In our study, an acute cell death generates the anticipated calcium uptake into the mitochondria, whereas hair cells undergoing a delayed cell death do not show any mitochondrial calcium spikes.
Moreover, mitochondrial calcium uptake is known to generate reactive oxygen species, which are damaging compounds for the cell. By using the mitochondria-targeted antioxidant mitoTEMPO, we can partially rescue neomycin toxicity. However, we see no protection against G418, suggesting that the mechanisms of hair cell death are different.
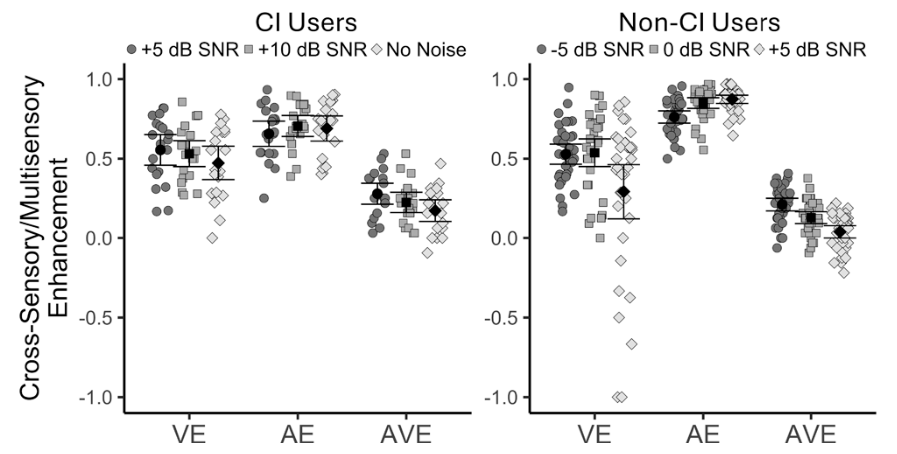
In the zebrafish model, a lysosome-disrupting treatment (GPN) protects hair cells from slow gentamicin damage but not from rapid neomycin damage. GPN significantly increased hair cell survival when given with gentamicin (A) but had no protective effect against neomycin (B). This suggests lysosomes are crucial in gentamicin's slower cell-killing process but not in neomycin's rapid damage pathway. Credit: Wu et al./Frontiers in Neurology
By fluorescently labeling the different aminoglycosides, we were able to track them inside the cell. We show that neomycin accumulates in two main compartments, the cytoplasm and lysosomes, whereas G418 appears almost completely inside lysosomes. This could suggest that lysosomes (cell cleanup centers) might play a role in the delayed hair cell death process.
One way to test this idea is by altering the lysosomal function. We found that by stressing the lysosome using the lysosome-disrupting small peptide, GPN, we can induce protection against a delayed cell death, while acute death is not sensitive to lysosomal manipulations.
Overall, our research shows the complexity of the hair cell response when exposed to closely related compounds. Moreover, it introduces the lysosome as a key role player during aminoglycoside-driven ototoxicity.
Our work will continue to deepen our understanding of the molecular pathways behind the process of aminoglycoside hair cell death, with the goal of devising future tools to prevent hearing loss from these and other ototoxic drugs.
A 2023–2024 Emerging Research Grants scientist, Francisco Barros-Becker, Ph.D., is a postdoctoral fellow at the University of Washington.
Los Antibióticos Dañan la Audición a Través de Diferentes Mecanismos
Por Francisco Barros-Becker, Ph.D.
Las células ciliadas mecanosensoriales desempeñan un papel fundamental durante el equilibrio y la audición. Desafortunadamente, muchos tipos de agresiones, como la exposición a ruidos fuertes o a ciertos medicamentos terapéuticos, pueden causar pérdida auditiva permanente al dañar o matar irreversiblemente estas células.
La clase de antibióticos aminoglucósidos son el estándar de atención para muchas infecciones bacterianas graves. Los estudios informan que la pérdida de audición por someterse a estos tratamientos (un efecto secundario conocido como ototoxicidad), puede oscilar entre el 11 y el 67 por ciento.
Comprender cómo estos medicamentos son capaces de matar las células ciliadas puede proporcionar nuevas vías terapéuticas potenciales para hacer que estos importantes medicamentos sean más seguros.
En nuestra publicación en Frontiers in Neurology de noviembre de 2024, exploramos cómo diferentes aminoglucósidos, como la neomicina y la gentamicina (o su análogo químico G418), son capaces de matar las células ciliadas de formas distintas. Usando el modelo de pez cebra, observamos que la neomicina puede destruir las células ciliadas de una manera aguda, y la mayoría de ellas desaparecen dentro de la primera hora después de la exposición al medicamento.
Por otro lado, la gentamicina o G418 mata de forma tardía, necesitando hasta 24 horas para generar una cantidad comparable de muerte de células ciliadas.
Una de las características previamente observadas de la muerte de las células ciliadas provocada por la neomicina es la rápida absorción de calcio mitocondrial que precede a la muerte de la célula ciliada. En nuestro estudio, una muerte celular aguda genera la absorción anticipada de calcio en las mitocondrias, mientras que las células ciliadas que experimentan una muerte celular tardía no muestran ningún pico de calcio mitocondrial.
Además, se sabe que la absorción de calcio mitocondrial genera especies reactivas de oxígeno, que son compuestos dañinos para la célula. Mediante el uso del antioxidante mitoTEMPO dirigido a las mitocondrias, podemos rescatar parcialmente la toxicidad de la neomicina. Sin embargo, no vemos ninguna protección contra el G418, lo que sugiere que los mecanismos de muerte de las células ciliadas son diferentes.
Mediante el marcado fluorescente de los diferentes aminoglucósidos, pudimos rastrearlos dentro de la célula. Demostramos que la neomicina se acumula en dos compartimentos principales, el citoplasma y los lisosomas, mientras que el G418 aparece casi por completo dentro de los lisosomas. Esto podría sugerir que los lisosomas (centros de limpieza de células), podrían desempeñar un papel en el proceso de muerte tardía de las células ciliadas.
Una forma de probar esta idea es alterando la función lisosomal. Descubrimos que al estresar el lisosoma utilizando el pequeño péptido disruptor de lisosomas, GPN (por sus siglas en inglés), podemos inducir protección contra una muerte celular retrasada, mientras que la muerte aguda no es sensible a las manipulaciones lisosomales.
En general, nuestra investigación muestra la complejidad de la respuesta de las células ciliadas cuando se exponen a compuestos estrechamente relacionados. Además, presenta al lisosoma como un actor clave durante la ototoxicidad impulsada por aminoglucósidos.
Nuestro trabajo continuará profundizando nuestra comprensión de las vías moleculares detrás del proceso de muerte de las células ciliadas por aminoglucósidos, con el objetivo de diseñar futuras herramientas para prevenir la pérdida de audición causada por estos y otros medicamentos ototóxicos.
Francisco Barros-Becker, Ph.D., científico beneficiario de las Becas de Investigación Emergente 2023-2024, es investigador postdoctoral en la Universidad de Washington.
Traducción al español realizada por Julio Flores-Alberca, julio 2025. Sepa más aquí.






For individuals with long-term hearing loss or severely degraded auditory input, the lack of reliable auditory feedback represents a challenge many orders of magnitude greater than the temporary masking used in this study.