By Emmeline Y. Lin, Stephanie M. Younan, MPH, Karen C. Barrett, Ph.D., and Nicole T. Jiam, M.D.
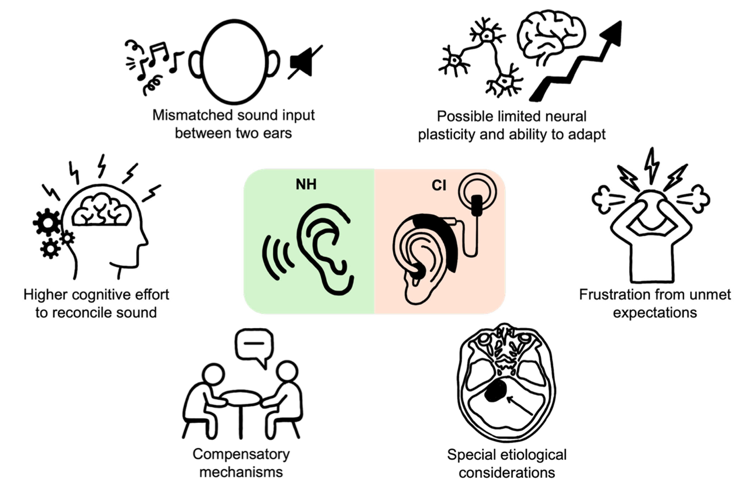
A new review explores the unique challenges faced by cochlear implant users with single-sided deafness—such as mismatched sound input between the ears and higher cognitive effort—and proposes a personalized approach to improve their outcomes and satisfaction. Credit: Lin et al./Journal of Personalized Medicine
Cochlear implants (CIs) are a modern marvel, restoring functional hearing for over a million people worldwide. While traditionally used for individuals with hearing loss in both ears, CIs are now an option for those with single-sided deafness (SSD), or profound hearing loss in one ear with typical hearing in the other. However, this group faces a unique challenge: Despite the potential benefits, patients with SSD often report lower satisfaction and use their implants less consistently than bilateral CI users.
The reason often comes down to the tale of two ears. For someone with SSD, their typical-hearing ear provides clear, sufficient sound in many quiet, daily situations, which can reduce the perceived need for the implant. Furthermore, the brain is tasked with fusing two very different signals: the natural, acoustic sound from one ear and the digitized, electrical sound from the CI. This mismatch can be jarring and cognitively demanding, leading some patients to simply turn their device off.
In our review published in the Journal of Personalized Medicine in September 2025, we argue that successfully treating SSD with a CI requires a fundamental shift away from the one-size-fits-all protocols used for bilateral hearing loss. We propose a personalized medicine framework that tailors care at every stage: pre-operative counseling, surgery, and post-surgical rehabilitation.
This personalized approach begins with counseling that sets realistic expectations, acknowledging that the CI will not perfectly replicate natural hearing. During surgery, techniques like individualized, anatomy-based frequency mapping can help minimize the jarring “place-pitch mismatch” between the two ears, a major source of dissatisfaction for SSD users.
After surgery, personalization is crucial for measuring success. Many SSD patients perform perfectly on standard speech-in-quiet tests due to their healthy ear, a “ceiling effect” that masks the real-world challenges they face. We propose using more sensitive metrics that assess sound quality and music perception. Because these aspects of hearing are far more acoustically complex than speech, they act as an ideal “stress test” for the auditory system, revealing the subtle processing deficits and distorted sound quality that drive frustration and guide more effective rehabilitation.
Looking forward, the future of personalized care lies in big data and machine learning. By creating large-scale registries of SSD patient data, we can train predictive models to forecast an individual’s likely outcome based on their unique clinical profile. This would transform counseling from providing general statistics to offering a data-driven, personalized prognosis.
Cochlear implants hold immense promise for the SSD population, but unlocking their full potential requires recognizing that these patients are not just half of a bilateral pair. By adopting a tailored framework, we can better address their unique challenges, improve consistent device use, and ultimately enhance their connection to the world of sound.
Study coauthor Emmeline Y. Lin (left, top) is a second-year medical student at Harvard Medical School. She received a B.S. in human biology from the University of Southern California.
Study coauthor Stephanie M. Younan (second from top) is a fourth-year medical student at the University of California, San Francisco. She received an MPH from Columbia University and a B.S. in physiological sciences from the University of California, Los Angeles.
Study coauthor Karen C. Barrett, Ph.D. (second from bottom), is a professor emerita in the department of otolaryngology–head and neck surgery and the Institute for Health & Aging at the University of California, San Francisco.
Study coauthor Nicole T. Jiam, M.D. (bottom), is a neurotology and skull base surgeon at the University of California, San Francisco. A 2024–2025 Emerging Research Grants scientist, she is the recipient of an Elizabeth M. Keithley, Ph.D. Early Stage Investigator Award, generously supported in part by Susan and Steve Kaufman. See summaries of two other recent papers by Jiam and colleagues: “Can Machine Learning Predict Who Will Benefit Most From Cochlear Implants?” and “Personalized Cochlear Implant Care Grounded in Music-Based Benchmarks.”








The internship last summer provided my first real chance to step into hearing science and learn the experimental side of speech perception under the tutelage of a senior researcher.