By Vijaya Prakash Krishnan Muthaiah, Ph.D.
Blast overpressure is responsible for 86 percent of U.S. service members wounded in action in Iraq and Afghanistan between 2001 and 2017. Many report post-concussive symptoms such as hearing loss, cochlear synaptopathy, tinnitus, hyperacusis, poor speech perception in noise, and cognitive deficits (such as learning, memory, attention, and emotional problems). Concerns have emerged about the long-term effects of mild traumatic brain injury (mTBI), a signature injury in blast explosions, to which an accelerated incidence of late-onset neurodegenerative disorders has been attributed.
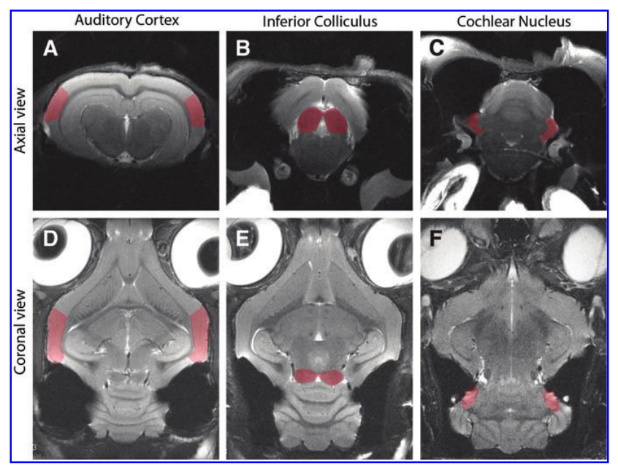
Specifically, the positive pressure phase of brief-duration blast overpressure inflicts mechanical damage to the cochlea and its central pathways, initiating a cascade of pathological cellular processes, primarily activation of oxidative mechanism and neuroinflammation, that result in neurodegeneration and cell death in the cochlea and higher auditory centers of the brain, such as the cochlear nucleus, inferior colliculus, and auditory cortex.
Evidence demonstrates that even a single-blast TBI can cause lasting neurological changes—without clinical symptoms—that are considered a risk factor for late-onset neurodegenerative disease, such as chronic traumatic encephalopathy (brain degeneration as a result of repeated head trauma). Researchers are investigating a potential association between tinnitus and dementia, for which there is some preliminary evidence.
Blast overpressure-induced conditions often overlap with post-traumatic stress disorder and chronic traumatic encephalopathy. In veterans, hearing loss and tinnitus are consistently rated as the top two service-connected disabilities, according to the Veterans Benefits Administration Annual Benefits Report for Fiscal Year 2020. However, due to the poor understanding of how tinnitus is caused and how it presents with the symptoms it does, there are to date no Food and Drug Administration-approved medications for tinnitus.
In addition, there are no evidence-based guidelines available for the definitive diagnosis, or directed treatment, of blast-induced mTBI. This too is due to a poor understanding of the underlying pathology, as few studies have focused on the unique lesions associated with blast overpressure. As a result it is critical to characterize and consolidate our understanding of blast-induced pathology in the central auditory neuraxis, or the auditory pathway in the higher brain centers.
For our study published in the Journal of Neurotrauma in November 2021, my team and I characterized blast-induced auditory neurodegeneration in the chinchilla, a widely adopted animal model in auditory neuroscience. Before delving into the molecular pathways underlying blast-induced pathology, we studied the structural changes using highly powerful 9.4T small animal diffusion tensor imaging (DTI) at the Center for Biomedical Imaging at the University at Buffalo.
Our results indicate that a single unilateral blast significantly impairs the structural and functional integrity at all levels of the central auditory neuraxis, or the auditory pathway in the higher brain centers. Overall, it is evident that the structural integrity of brain tissue is compromised at all levels. Credit: Krishnan Muthaiah et al./Journal of Neurotrauma
Our investigation is the first of its kind to perform DTI in the chinchilla. DTI is a powerful technique for monitoring the response of the brain to trauma. In this study, the tissue microstructure of the auditory pathway was probed using a quantitative and noninvasive magnetic resonance DTI approach to collect images of water diffusion properties in auditory higher centers.
The water diffusion in tissues is highly sensitive to differences in the microstructural architecture of cellular membranes, making it a powerful method for detecting microscopic differences in tissue properties. Thus, the quantitative scalar DTI metrics are directly linked to the anatomic organization and microstructural features of white matter fiber tracts in the central auditory neuraxis.
This study’s findings are more generalizable to humans for two reasons: 1) The chinchilla has a hearing range and size of tissue microstructure similar to humans; and 2) the measures used to probe the pathophysiological changes (such as auditory brainstem response, or ABR, and neuroimaging) are commonly applied to humans as well.
Our results indicate that a single unilateral blast significantly impairs the structural and functional integrity at all levels of the central auditory neuraxis. Overall, it is evident that the cytoarchitecture, the structural integrity of brain tissue, is compromised at all levels, particularly at the cochlear nucleus and auditory cortex.
Vijaya Prakash Krishnan Muthaiah, Ph.D., is an assistant professor in the department of rehabilitation sciences at the University at Buffalo, the State University of New York. His 2019 Emerging Research Grant was generously funded by the General Grand Chapter Royal Arch Masons International.







The internship last summer provided my first real chance to step into hearing science and learn the experimental side of speech perception under the tutelage of a senior researcher.