By Alexander Chern, M.D., and Anil K. Lalwani, M.D.
As of September 2020, the coronavirus COVID-19 pandemic caused by the SARS-CoV-2 virus has caused nearly 33 million cases and almost 1 million reported deaths worldwide since first identified in Wuhan, China. How the disease appears can vary, ranging from mild upper respiratory symptoms to more severe complications of acute respiratory distress syndrome, pneumonia, multiple organ failure, and even death. As clinicians and scientists continue to study and characterize this novel disease, reports of unusual symptoms and manifestations of COVID-19 have begun to arise.
As such, in the journal Otology & Neurology on Sept. 4, 2020, we reported a case of an 18-year-old woman who arrived as a patient in our clinic with seven weeks of sudden hearing loss in both ears, intermittent aural fullness (sensation of clogged ears), and vertigo. Her hearing test showed a moderate to severe sensorineural hearing loss in the right ear, and a moderate to profound sensorineural hearing loss in the left ear.
Laboratory testing performed several weeks after her initial visit was positive for IgG COVID-19 antibodies; this suggests her COVID-19 infection most likely coincided with the onset of her hearing loss several weeks before presenting to our clinic. Her magnetic resonance imaging (MRI) demonstrated intralabyrinthine hemorrhage (inner ear bleeding) in both ears. After undergoing steroid therapy, her hearing and vestibular symptoms improved.
As clinicians and scientists continue to study and characterize COVID-19, reports of unusual symptoms and manifestations of the disease, including sudden hearing loss, have begun to arise.
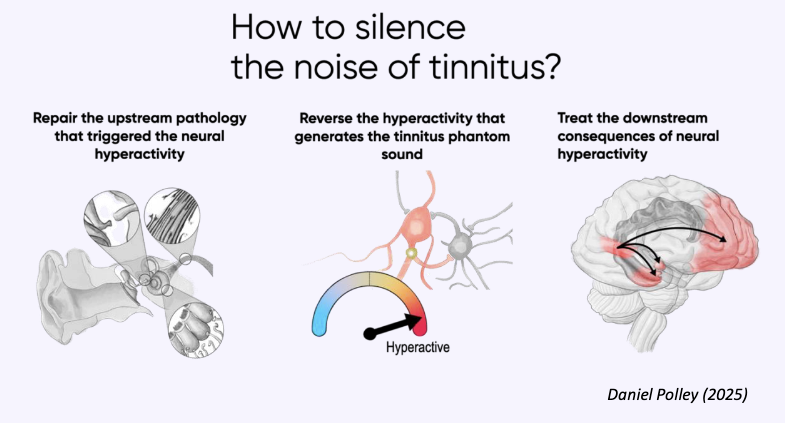
Although there are previous anecdotal reports, this is the first well-documented case of sudden sensorineural hearing loss in a patient with COVID-19. There is strong evidence that viral infections can cause sudden sensorineural hearing loss, which implicates the SARS-CoV-2 virus as the cause of the patient’s hearing loss. Intralabyrinthine hemorrhages can cause hearing loss from disruption of the microcirculation of the inner ear, which can interfere with mechanisms essential for normal hearing function, including the endocochlear potential, ion transport, and endolymphatic fluid balance.
COVID-19 is actually thought to cause vascular changes in the body, such as injury to blood vessels and widespread micro-clots, which are thought to underlie the acute respiratory failure and multiple organ dysfunction (e.g., the brain and the heart) in some patients with the disease. From this case, we conclude that COVID-19 can affect the inner ear.
In medicine, a case report comprises a detailed account of the symptoms, signs, diagnosis, treatment, and follow-up of a patient. Case reports typically describe unusual or novel manifestations of a disease, and remain a cornerstone of medical progress—improved patient outcomes result from studies and investigations that have been conducted based on valuable information and new ideas presented by case reports. Sir William Osler, one of the founding fathers of modern medicine, once said, “Always note and record the unusual… Publish it. Save it on a permanent record as a short, concise note. Such communications are always of value.” As physicians and researchers become more familiar with the COVID-19 disease process and how it may affect patients, it is important to report novel findings and their experience with the disease.
Sudden hearing loss is an unusual and previously undescribed symptom of COVID-19 that is particularly important to us as otolaryngologists (also known as ear, nose, and throat specialists, or ENTs). We, along with our audiology and speech language pathology colleagues, hold special roles as gatekeepers and guardians of communication.
This specific manifestation of COVID-19 dovetails with the known communication barriers caused by consequences of the COVID-19 pandemic, such as mask wearing, social distancing, and virtual meetings. Characterizing and reporting the manifestations and consequences of the COVID-19 will be crucial for developing strategies to mitigate the impact of the COVID-19 pandemic on society.
My name is Alex Chern—I am a third-year resident physician in otolaryngology–head & neck surgery (ear, nose, and throat surgery) at NewYork-Presbyterian (Columbia and Weill Cornell). I am also a musician (violinist) with a hearing loss treated with hearing aids, and have contributed to Hearing Health magazine and the HHF blog.
I am collaborating on another study with Anil Lalwani, M.D., the head of HHF’s Council of Scientific Trustees and member of HHF’s Board of Directors, and a professor and vice chair for research in the division of otology, neurology, and skull base surgery at Columbia University.
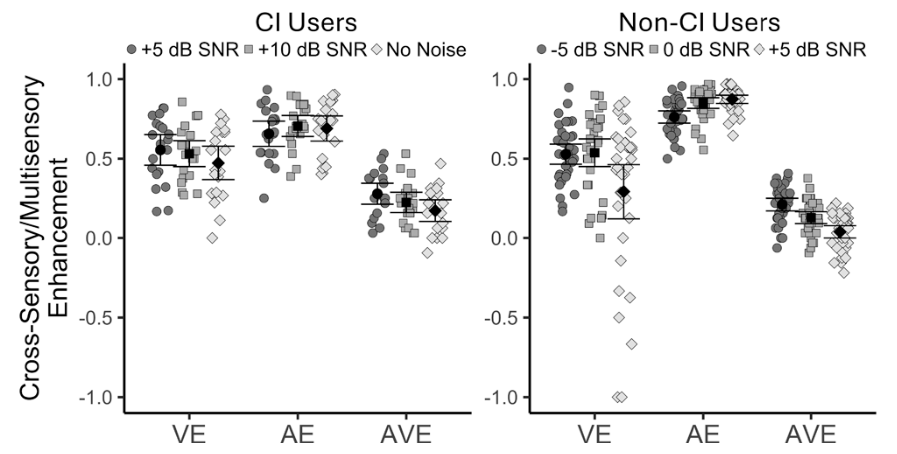
We are examining the effect of hearing loss on music enjoyment and are actively recruiting individuals with bilateral hearing aids (a hearing aid in each ear) to complete a 20- to 30-minute online study. The study involves listening to music on your computer and answering questions about them. No headphones or other special equipment is required.
Please contact alc9230@nyp.org if you are interested. Thank you very much.






We are proud that Hearing Health Foundation-funded scientists are always well represented at Association for Research in Otolaryngology MidWinter Meeting.