What Is Ménière’s Disease?
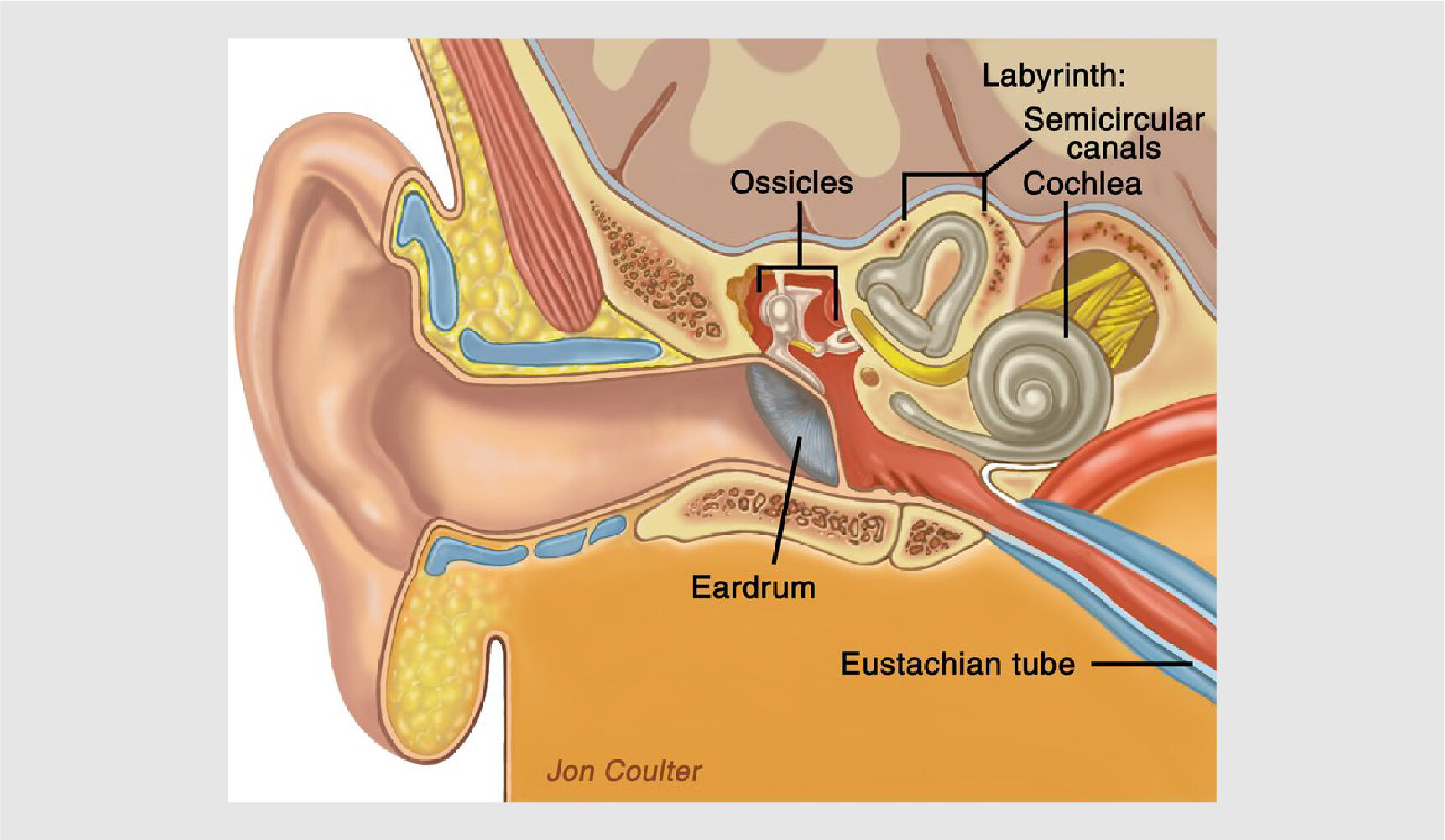
Ménière’s disease is a chronic inner ear disorder affecting balance and hearing.
French doctor Prosper Ménière first identified and described the symptoms of the medical condition that now bears his name in 1861. These symptoms include fluctuating hearing loss, episodic vertigo, a sensation of ear fullness, and tinnitus.
Many disorders have similar characteristics.
In its 2020 clinical practice guideline, the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) uses this definition:
“Ménière’s disease is a disorder of the inner ear that includes episodes of vertigo with possible hearing loss, ringing or buzzing in the ear, or ear pressure.
“Ménière’s disease is defined by spontaneous vertigo attacks, each lasting 20 minutes to 12 hours, with low- to mid-frequency sensorineural hearing loss in the affected ear before, during, or after one of the episodes of vertigo. The clinical practice guideline defines vertigo as the feeling of spinning or moving when one is not moving. This is different from dizziness, which can mean feeling lightheaded or feeling like passing out.”
Most cases are in one ear and in adults ages 40 to 50.
Most cases of Ménière’s disease are unilateral (affecting only one ear), but some will be affected in both ears. Ménière’s disease often starts as unilateral and progresses to bilateral. Around 15 percent of people with Ménière’s will experience bilateral hearing loss.
It's estimated that there are 600,000–750,000 cases of Ménière’s disease in the United States, with 45,000 to 60,000 new cases diagnosed annually. Estimates of the worldwide incidence of Ménière’s disease vary significantly, from 3.5 to 513 per 100,000.
According to AAO-HNS, “Ménière’s disease is almost exclusively reported in adults, with less than 3 percent of cases estimated to occur in children younger than 18 years old. The disease is most prevalent between ages 40 to 60 years, with peak onset in the 40s and 50s.
“In many patients, the most detrimental decline in hearing and balance function occurs within the first decade of diagnosis, yet patients continue to have longstanding deficits that make Ménière’s disease a chronic disease. It is important to evaluate and document the hearing in both ears as a subset of patients will eventually experience Ménière’s disease bilaterally.”
Learn More:
What Is Ménière’s Disease?
Causes
Symptoms and Diagnosis
Treatment
How Balance Works
Our Research on Ménière’s Disease














Eventually I told my boss that I would have to resign. As it turns out, that was the best decision I could have made. The enormous stress of my job had been a large contributing factor to the severity of my disease, and letting that responsibility go was decidedly the medicine I needed.